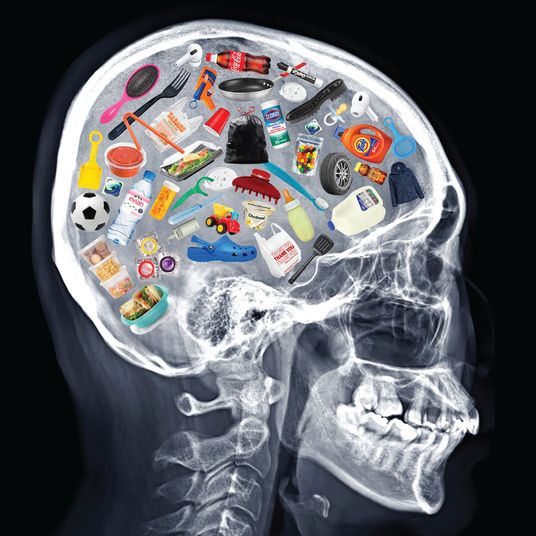
At first brush, the COVID-19 crisis looked like it was designed in a lab — to lay bare the insanity of the American health-care system.
Employer-provided insurance has always been a bizarre and retrograde practice that’s earned our people a reputation for barbarism among more enlightened civilizations. But a pandemic-induced recession threw the perversity of the American way of health care into stark relief: Who could defend tying medical coverage to full-time employment when tens of millions were losing their jobs to a public-health catastrophe?
Similarly, financing hospitals on a fee-for-service model — such that lifeline institutions in poor, rural regions struggle to remain open while those in affluent, urban areas indulge in needless renovations and extravagant executive compensation — had always been a cruel joke. But as the pandemic choked off hospital revenue while simultaneously ramping up need, it became gallows humor. Seeking to curb medical inflation — without curtailing elite health-care professionals’ outsize incomes — by gutting hospitals’ surge capacity and discouraging the disempowered from visiting the doctor through high-deductible plans was always injurious; in 2020, it became patently murderous.
The ideologically inclined are famous for seeing every crisis as a validation of what they’ve always believed. But polling lent credence to the left’s sense of vindication: Within weeks of the pandemic’s onset, Morning Consult registered a double-digit increase in public support for Medicare for All.
But neither strong arguments nor opinion polls make policy in the United States. Organized interest groups and political parties do. And far from eroding the political power of the health-care industry’s incumbent rentiers, the pandemic lent hospital and physician lobbies a new degree of social esteem. Meanwhile, Democratic primary voters’ decision to nominate the 2020 candidate with the most limited ambitions for expanding public health insurance — combined with the general electorate’s decision to thin Nancy Pelosi’s House majority and leave the Senate balanced on a knife’s edge — dimmed the prospects for major health reform at the federal level in 2021.
More maddeningly, the pandemic actually reversed progress toward expanding public health insurance in states. In early January, the Democratic governor of Kansas Laura Kelly and the state’s Republican leadership struck a deal that would have expanded Medicaid coverage to 150,000 Kansans. Then COVID ripped a $600 million hole in the state’s budget. Now, the Medicaid expansion deal appears “all but dead.” “If there is some additional cash available, it needs to go to small businesses,” incoming state Senate Majority Leader Gene Suellentrop told Politico this week. “That’s going to get the most benefit to the most people.” In North Carolina, pandemic-induced budget concerns have fortified Republican opposition to Democratic governor Roy Cooper’s Medicaid expansion plans.
The setbacks extend to blue states, where unified Democratic governments have tempered plans for expanding public health insurance. Colorado Democrats began the year with ambitions to establish a strong public option for health insurance in the state, one that would force doctors and hospitals to accept lower payment rates than private insurers provide. Then the pandemic exhausted the party’s already-limited appetite for taking on hospital and physician lobbies, which wasted no time in arguing that support for a public insurance option was tantamount to undermining “our front-line workers and facilities that are essential to pandemic response.”
Now, the public option’s strongest supporters in the state legislature are trying to save their proposal by neutering it, allowing hospitals to refuse to accept the public option as valid insurance. Even with this concession, the bill’s sponsor told Politico that its odds of passage are looking dicey.
In Washington, industry pressure led Democrats to make that state’s public option voluntary for hospitals, even before the pandemic hit. In COVID’s wake, it restricted implementation of this weak public option to just one-third of the state’s counties. Enrollment in the public option has been underwhelming, in part because — thanks to Democrats’ concessions on payment rates — the public plan isn’t consistently outcompeting private insurers on price. It is possible to institute a public option that delivers truly affordable health insurance for its enrollees without eating into hospitals’ profits and doctors’ incomes, but only by heavily subsidizing the public option’s cost. Alas, due to the COVID crisis, and Congress’s failure to send unconditional fiscal aid to states, Washington Democrats feel that they “don’t have the money to put in more subsidies.”
Given the Republican Party’s structural overrepresentation at the federal level, there is a strong case for health-justice advocates to focus on winning major reforms in states. It is true that there are unique challenges to implementing a strong public option or single-payer system at the state level. Unlike the federal government, individual U.S. states cannot print their own currencies, and high-income taxpayers and medical professionals have some ability to relocate in response to reforms that cut aggressively against their interests. Nevertheless, California boasts an economy larger than that of many European nations that share the Golden State’s lack of monetary sovereignty — but still manage to provide affordable health insurance to all residents. Were California, Washington, and Oregon to coordinate on health-care reform, the threat of inducing doctor and/or high-income taxpayer flight through progressive reform would be further diminished. What’s more, if progressives were able to stand up an enviable state-level model for universal coverage — that actually reduced the cost of business for most firms by slashing their health-care expenses — that would likely weaken the position of their movement’s opponents in both D.C. and redder states.
To regain momentum lost to the pandemic, however, proponents of public health insurance will need to secure enough fiscal aid to states to ease budgetary pressures; it is hard to win large increases in social spending when state governments can’t afford their existing outlays. If Democrats sweep next week’s Senate runoff elections in Georgia, the party will have the power to make all manner of state-level social-democratic reforms more feasible; progressives must fight to ensure the party uses that power to the fullest. Precisely how reformers can go about eroding the cultural and political influence of health-care industry lobbies is less clear-cut. But the more power state governments have to subsidize public-option plans and financially insecure hospitals, the less capacity industry groups will have to nip reform efforts in the bud.
In sum: COVID has made the sickness of America’s health-care system more apparent. But it’s brought our political leaders no closer to approving invasive treatment for that pathology. Successful trials in our “laboratories of democracy” might change that — but only if the funding for such experiments comes through.