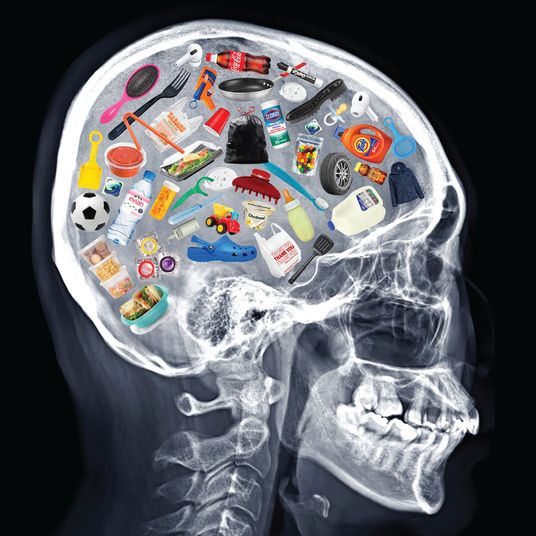
Almost as soon as scientists began working on vaccines against COVID-19, public-health experts began to worry about “vaccine hesitancy,” the refusal or reluctance of people to get a shot. While the U.S. vaccination program is a roaring success judging by the more than 3 million shots administered each day, hesitancy has been considered a threat to the goal of inoculating enough people to achieve herd immunity and tame the coronavirus once and for all.
Those fears about the problem of hesitancy have been heightened following reports of rare but serious blood clots in at least six women who received the Johnson & Johnson shot out of a total of 7 million people. Federal regulators paused the shot “out of an abundance of caution” on Tuesday and convened an emergency meeting of experts on Wednesday to study the phenomenon. “We believe these events to be extremely rare,” CDC director Dr. Rochelle Walensky said in a White House press briefing before the meeting. “But we are also not yet certain we have heard about all possible cases, as this syndrome may not be easily recognized as one associated with the vaccine.”
Early data from an Economist/YouGov poll suggests the news of the clots and the decision to pause may have dented public perception on the vaccine. Before the announcement, 52 percent of those surveyed thought the shot was safe; after, that dropped by 15 percentage points to 37 percent.
A similar response was seen in Europe after several nations paused the AstraZeneca vaccine over the same fear of clots in the brain of people who got that shot. The two may be linked: AstraZeneca and Johnson & Johnson’s shots use the same type of harmless virus, unlike Pfizer and Moderna’s shots. AstraZeneca’s vaccine has not yet been approved for use in the U.S. In mid-March, after France paused the AstraZeneca shot, a poll suggested that only 20 percent of those surveyed said they trusted that vaccine, compared to 52 percent who expressed confidence in Pfizer’s shot.
Similar wariness was found across the Continent. Michael Bang Peterson, a political scientist at Aarhus University in Denmark, one of the first countries to suspend the AstraZeneca shot, surveyed a representative sample of people in eight European Union countries and found confidence in any vaccine dropped by about 11 percentage points in Denmark immediately after the shot was suspended in mid-March. (In a world first, Denmark ditched the AstraZeneca shot altogether on Wednesday.) In other countries, such as Sweden and Italy, Peterson’s study found vaccine confidence also slipped but by about 5 points following reports about the vaccine and clots. Confidence decreased further when those countries themselves suspended the shot, Peterson and researchers found. (Peterson’s study has not yet been published in a scientific journal or peer-reviewed.)
“We have only seen very small changes, perhaps a few percentage points as a consequence of the Astra-Zeneca turmoil,” Peterson told Intelligencer. “It seems the pause introduces uncertainty but doesn’t necessarily lead people to have a strong rejection of the vaccination program overall.”
Peterson said he is currently doing research on how best to communicate negative information about vaccines, like low efficacy and side effects. ”What the research is suggesting is that it’s crucial that health authorities communicate as transparently as possible, even about things that may be a cause of concern and anxiety for the public.”
One of the things that undergirds vaccine acceptance is public trust in health authorities. “While you can induce people to be worried about the shot, you can increase trust in the communicator,” he said. “You may lose the short-term battle, because you are inducing uncertainty toward the vaccine. But then you are in a position to win the long-term war” against the virus.
On this side of the Atlantic, polling suggests vaccine hesitancy had declined before the Johnson & Johnson pause, following public-health efforts to reassure people about the vaccine’s safety. In a March survey by the Kaiser Family Foundation, 55 percent of Black respondents said they wanted the vaccine as soon as possible or were already vaccinated. Twenty-four percent were still holding back to wait and see about the vaccine’s effects, down from 52 percent in December. Hesitancy to get a vaccine remains high among Republicans and white Evangelical Christians: In an Economist-YouGov poll released last week, 40 percent of Republican voters and 38 percent of former Donald Trump supporters said they would not get a vaccine even when offered one.
Stefanie Friedhoff, faculty member at Brown University’s School of Public Health, cautioned there are limits to polling the phenomenon of vaccine hesitancy. “They can be confusing because they don’t tell us anything about people’s realities on the ground,” and it “distracts from some important underlying reasons for why people aren’t getting it.”
Friedhoff, who is also a health-care journalist, is skeptical of how useful the concept is for explaining low uptake of vaccines.
“We sometimes rush into a narrative of immediately interpreting everything through the lens of vaccine hesitancy,” she said. “It’s become a catchall term that describes sort of a whole subset of issues,” such as lack of access and misinformation, not individual choices.
So far, it’s unclear when the Johnson & Johnson pause may end. After four hours of questions and presentations on Wednesday, the CDC’s Advisory Committee on Immunization Practices said it needs more time to study reports of clots to consider whether to recommend the shot’s continued use, effectively extending the pause.