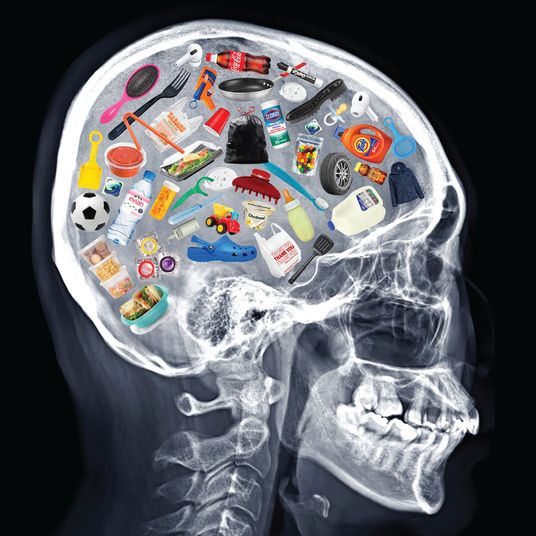
The day my phone rang last week was unusual in that I had not yet Googled “when can kids get the COVID vaxx,” “pediatric vaccine timeline,” or some combination thereof, despite having been awake for hours. It hadn’t been necessary: Fellow despairing parents of those too young to be vaccinated had already filled my social-media feeds with the latest, grimmest headlines.
The nearly sevenfold increase in new COVID infections among children between the first week of July and the first week of August, and then the 48 percent rise in the week that followed; the pediatric ICUs at or near capacity in states with low vaccination rates; the desperate hope that the FDA providing full approval to Pfizer’s vaccine would allow pediatricians to prescribe it off-label to the under-12 set — 48 million people — for whom trials are still underway. On Monday, both the FDA commissioner and the American Academy of Pediatrics firmly discouraged this ad-hoc option, though the AAP has previously told the FDA to hurry up on kids’ vaccines. The anticipated timeline has hovered in the realm of vagueness; on Tuesday, Fauci said “hopefully by the mid-late fall and early winter,” whatever that means. In the meantime, teachers and parents alike looked to the start of the school year with fresh dread.
In early July, I read that vaccine-makers were increasing the size of their trials for kids, at the request of the FDA. It took only a few minutes to figure out where to sign up, which involved volunteering information on suspiciously generic forms on third-party sites to try to get on what was doubtless a thousands-long wait list. We’d have to drive several hours to the nearest Pfizer or Moderna trial site — according to websites that looked as though they could possibly be part of a phishing scam — but we have a car, and signing up was free.
When my phone rang last Wednesday evening — a Minnesota number I didn’t recognize — I answered out of reportorial reflex. The guy, who sounded like a 30-something bro, said he was calling on behalf of a pediatric COVID-vaccine trial. Was I still interested in enrolling my child?
I frantically motioned for my husband to come over and put Minnesota (whose title, I would later learn, was “remote clinical research coordinator”) on speakerphone. The caller wanted to confirm my daughter’s age (14 months) and whether she had any immune issues (she does not). He explained that two-thirds of the recipients would receive the actual vaccine, and that one-third would get a placebo; he said those in the latter group would find out at either the six-month mark or when there was an emergency-use authorization, whichever came first. I’ve never been a numbers person, but this seemed like pretty good odds.
“The only thing is,” said Minnesota, “it would have to be tomorrow at 9 a.m. or 2:30 p.m.”
Next to me, my husband, who has a finely tuned sensor for schlep, frowned. “We’re doing it,” I scream-whispered.
Minnesota wasn’t finished. “Oh, and it’s in …” He named a town that sounded, aptly enough, more like a pharmaceutical cocktail than a place.
At this, I did hesitate. “What state is that?”
He didn’t know either.
Whatever, as long as we could make it in time for our appointment. I had no doubt it was worth it. Though the mantra has long been that children are low-risk and pediatric deaths remain a tiny percentage of the overall total, Delta’s infectiousness — and, perhaps, virulence — has shaken that assumption. The long-term unknowns of kids getting COVID scare me much more than a phase-two trial conducted under supervision. Pfizer and Moderna began testing the vaccine on kids under 12 in March, using a reduced dosage by age, and surely the trials would have been stopped if there’d been any problem. And while scientists are still trying to parse what Delta means for vaccine efficacy, lowering the chance of infection and transmission to my daughter’s high-risk grandparents was, to me, reason enough.
We hung up with Minnesota just after 5 p.m. By 8 p.m., blessed with personal and professional flexibility, we were loading a sleepy toddler into the car to drive for as long as we could. In the breathless interim, we’d figured out the drive would take between six and eight hours and that even with the later appointment, it would make sense to break up the journey.
We stopped at midnight. No one slept much that night, least of all the toddler, for whom being born in stay-at-home times has meant seldom breaking the routine. The next day, we still had nearly three hours to go, and a steady drip of Bamba snacks and Moana YouTube clips was at most harm reduction.
The study site was in a family-practice office adjacent to a research hospital, an ordinary doctor’s office with nurses who wore pink K95s. I had imagined a room of crying infants waiting their turn but only saw one other baby. It felt eerily casual, like a regular checkup but with more forms to sign and a longer-than-usual ordeal (two and a half hours in the exam room, including monitoring time) — and this time, we were asked if we were a direct descendant of anyone at Pfizer.
“New York!” more than one of the researchers said in faint surprise, as if they wondered why we’d bothered. “Wasn’t there a study site closer to you?” Then again, the study doctor shrugged, “We aren’t struggling to enroll people.” Our spot had opened up because someone had canceled at the last minute.
The night before, I’d managed to skim the dozens of pages on the consent form. Phase one of the study had experimented with three different dosages, “to see which dose level is safe and makes the most antibodies.” Everyone in that phase got the real thing. In phase two to three, which is where we came in, researchers were looking for broader safety information, and blood samples would tell how many antibodies the kids were making. Only the person giving the injection would know whether we were in the unlucky one-third to get the placebo. There were 4,500 kids in this phase, at 100 different sites, ranging in age from 6 months old to 11, all of them bound together by science and opportunity. We’ve committed to between 5 and 11 of these visits over the next two years, partly depending on whether we got the placebo or not; for each one, we get paid $120, roughly the cost of one night in the roadside TownePlace Suites where we slept.
My daughter was only a few months old when she started locking eyes with us in shocked betrayal every time we took her to the doctor. This time, I held her for the nose swab and what felt like a 30-minute blood draw (it was probably more like two). In went the injection, whatever it was, in her upper thigh, and on went two rainbow Band-Aids.
Since then, we’ve taken her temperature — at this age, it’s rectal, for which we hope to be forgiven someday — and I log it and answer questions about how she’s doing on an app. So far, there’s no swelling and no redness at the injection site, no fever, no irritability, no loss of appetite. The temperature checks last for seven days after each shot, and the weekly log of any possible COVID symptoms is up to a two-year commitment.
Of course, now I have something new to worry about: whether her lack of symptoms signal what was in that syringe. Babies are getting a smaller dose (three μ, a tenth of what adults get in a unit I’ve never before encountered), and some adults didn’t have any side effects at all. Either way, I have no regrets. We all have our risk calculations, our hierarchy of fears, our coping strategies. I’ve started asking that everyone we see indoors take a rapid test, even when they’re hard to find in stock. We stay home as much as possible and feel guiltily relieved that our daughter is too young to need school. Some parents have coached their 11-year-olds to lie about their ages in order to qualify for the vaccine; some are homeschooling or moving to entirely new places to feel safer; some are gritting their teeth and hoping for the best. None of us can do much to make the eligible unvaccinated get the fucking shot already, and it is inevitable that these same people and more will be demagoguing their kids’ immunization as soon as it’s an option. There’s not that much I can do about any of it, but I can do this.