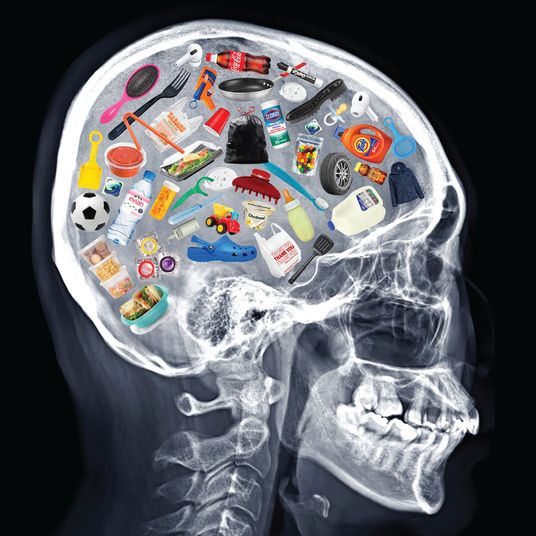
Editor’s note: The following account comes from a New Yorker, age 78, who has a chronic illness requiring regular injections of Humira, a drug that suppresses the immune system. He is therefore more vulnerable to COVID-19 than most people and less able to respond to vaccination and thus build immunity. After receiving a standard two-shot dose of Moderna’s vaccine earlier this year, two weeks ago he received an underground third dose of Johnson & Johnson’s single shot, a treatment that has not been approved by federal regulators who are studying whether so-called boosters should be administered.
I got the first two shots in January and early February. It was the Moderna vaccine, and I had no symptoms or reaction. In April or May, I saw my gastroenterologist — who prescribes a medication, Humira, that is hostile to the immune system — and he asked me if I wanted to be tested for the vaccine’s efficacy because he was doing an informal study. The results came back for two different tests not indicating any immunity. And, you know, he talked to me and said not to get upset about it and that there are other ways of measuring efficacy. These tests were roughly the same ones used in the trials. When they did the trials, they deliberately excluded people who were immunocompromised — they had to! They would have to set aside a placebo group, and they didn’t want to kill ’em. So that population is in the shadows. The people who should be really concerned are transplant people — mine is just a drug that attacks one aspect of immunity. They’re really potentially at risk.
I don’t remember which of us brought up the idea of an extra shot. My gastroenterologist said he was not permitted to authorize it but would support it if I tried. He didn’t suggest I do it then — it was “wait and see what happens” — and I didn’t go for it right away. It was early in the spring when he ran this test, and we hadn’t finished giving a lot of shots and we didn’t have the Delta variant. My rheumatologist, who is concerned — they talk to each other — spoke to [a hospital administrator] who said, “We’re not recommending this at this point.” In other words, she talked to the bureaucrat. But she’s a doer.
The gastro people recommended that I get it halfway between my Humira injections, which are every two weeks, because the Humira wears off gradually. But you don’t want it too close to your next dose in case the Humira shots themselves interfere with the response to the vaccine. We don’t know that that happens, but we suspect it.
I wanted to get the Pfizer vaccine, and I was in another state, not New York, last month. I didn’t lie. The people at the hospital system there are really good — well organized. They had me in the same computer system and asked me whether I’ve had shots, and I said, “Yes, but they didn’t take,” and they said, “You can’t have it.” I waited for another break from the Humira a month later and went to a pharmacy, which I knew would be sloppy. They didn’t ask. And I don’t know if the states all plug into the CDC, but I knew the pharmacy wasn’t going to be using any databases. They gave me the one-shot J&J. I haven’t been tested since — I suspect the doctor will test me in the fall.
I had a few aches and pains after the third shot, but it’s difficult at age 78 to determine the source of an ache. We moved the couch the other day — I might blame the couch.
I didn’t take anything away from anyone. If I had done this in March, there were people who were desperate waiting on line. Now, you can’t give it away. And what I did will soon be available and encouraged: Francis Collins, the head of the CDC, said this is not a booster shot — this is attempting to get the first shots right. And that’s right.