From abroad, where COVID-conscious Americans now look for portents of our near-term Omicron future, nearly all the signs have been positive over the last few weeks. In fact, case numbers aside, the U.K. and continental surges and new research from labs in Japan and Liverpool and Cambridge and Hong Kong (among other places) have made Omicron look almost like a best-case scenario or at least what would’ve qualified as one just a few weeks ago, once we knew how quickly the wave was spreading but not yet how quickly the wave would subside or how much severe disease would be left in its wake.
In all of these places, initial case growth was dizzying — if earlier surges were defined by exponential growth, with Omicron it seemed practically stratospheric. But the waves turned quickly — in South Africa, cases peaked just four weeks after the wave began, and in London, the wave has turned now too. In South Africa, the picture of severity was even more encouraging, since COVID fatalities there reached only a fraction of the level reached at the height of the country’s previous wave (in some charts you couldn’t even see a rise in excess mortality). In the U.K., where hospitalizations are still growing, especially among the elderly, the death toll is likely to be more significant, though still well below the levels reached by the country last winter. This reduced severity is no mystery — study after study is now demonstrating that Omicron is much less effective in the lungs, where it can do the most damage, than previous variants. And several small-scale studies have suggested that — despite early concerns that Omicron’s capacity for reinfection and breakthroughs meant it might not produce much “cross-protection” against other variants — infection with the new variant probably does offer enough cross-protection that a true “parallel pandemic” is an unlikely outcome.
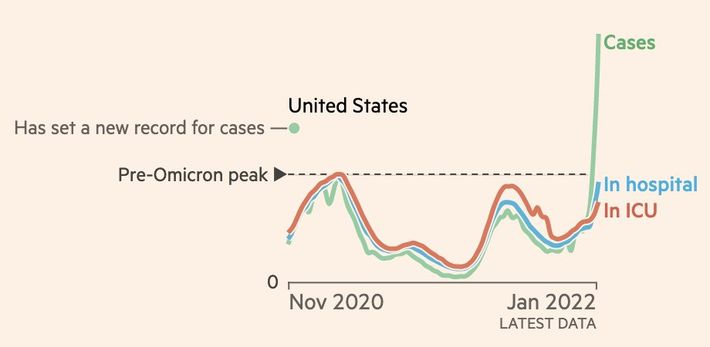
But while this is all encouraging, it is not clear that those same patterns observed abroad will hold here in the U.S. In fact, there are already early signs in hospitalization and ICU data that the experience of Omicron in America may be harsher than has been observed so far in Europe. This should perhaps not come as a surprise, given that Delta was much more lethal in the U.S. than in Europe — and the current data may still reflect some lingering cases of that variant. And it does not mean a tsunami of deaths is right around the corner or that this new variant will mean for the U.S. what Delta meant for India. (To begin with, the U.S. is, by global standards, very well vaccinated.) But the higher rate of severity observed so far is a reminder that the shape of a pandemic is not simply a matter of the biological properties of the virus; it is also determined by the social and immunological context in which that virus spreads. And it appears that, with Omicron as with Delta, the American context may be different enough to make a real difference, delivering perhaps considerably more severe illness and death than we’ve seen on the other side of the Atlantic.
With Delta, many Americans observed a miraculously light British wave and effectively ignored the real carnage that followed here — 100,000 Americans dead, and September and October was the deadliest two-month phase of the pandemic outside of last winter’s horrific surge. With Omicron, the same pattern — optimism from Europe followed by overlooked suffering here — seems troublingly possible again. And if you’re hoping for an outcome resembling South Africa’s, where COVID deaths during the Omicron wave didn’t reach even 10 percent of the previous peak, keep in mind that the U.S. began this wave on a Delta plateau 50 percent as high as our previous peak of daily deaths.
To this point in the Omicron surge, at least, American fatalities have not grown dramatically from that plateau, and the small rise we have observed is as likely to be the result of ongoing Delta cases as Omicron infections (that is how fast this surge has come upon us — our data are still telling a story about the last one). Anecdotal reporting from around the country suggests that while new patients are crowding hospitals and emergency rooms, to the doctors working in those hospitals the Omicron cases appear, on the whole, less serious. But while the New York Times reported this week this wave is putting less pressure on ICUs than previous ones, state data tell a different story: A comparable proportion of hospitalized cases are already now in the ICU as was the case in New York during the winter surge of early 2021. Then, hospital admissions reached 9,000; now, we’re already past 10,000. ICU admissions got to 1,600; now, we’re at 1,404.
And the numbers are still growing, quite fast. NYU epidemiologist Celine Gounder told me that between December 27 and January 3, ICU admissions in the city as a whole grew 55 percent. “That is not a small jump,” she said. It took place in just a week. Statewide, on the day before Christmas there were 4,891 COVID-19 patients hospitalized, 880 of them in the ICU; yesterday, there were 11,184 in total, with 1,404 in the ICU. In less than two weeks, in other words, hospitalizations had more than doubled and ICU admissions had grown by 60 percent. Cases had grown a lot too, from 49,708 on Christmas Eve to 84,202 yesterday. But a 70 percent jump in cases accompanied by a 60 percent jump in ICU admissions does not suggest a dramatic “decoupling” of the kind we’ve observed in South Africa and Europe and seemed almost trying to will into existence here. And since, in general, hospitalization surges lag behind case surges, it is worth keeping in mind that the data we have now about hospitalization levels all reflect infections from the Omicron upswing, not its peak, which may well be ahead of us. Gounder says she expects another week or two before a local peak here in New York, followed by another week or two before we reach a national peak — a rough timetable echoed Thursday by the epidemiological modeler Jeffrey Shaman. But already the country is reporting more than half a million new cases every day; the new daily case counts are rapidly approaching one million, four times as high as the worst days of the surge last winter.
“This is the point I’ve made over and over,” Gounder says. “The simple math I give is even if it’s half as virulent — so half as deadly, your case fatality rate is reduced by half — if you have twice as many cases, you have actually the exact same number of deaths.” The way other concerned doctors and epidemiologists have put it is: A small fraction of a huge number is still a large number.
“I think people have fixated on this idea that it’s mild,” Gounder says. “Mild means mild — relatively mild — for the individual who’s infected. But it does not necessarily mean mild at a population level in terms of numbers of deaths. If a lot of people get infected, even if it’s a relatively benign virus, enough of those people will still have to be hospitalized and die that this is really going to be very overwhelming for the health-care system. I think it’s gonna be really tragic.”
“I’m very reluctant to quote, unquote, ‘learn’ anything from what South Africa and the U.K. experienced,” says Brigham and Women’s Hospital emergency physician Jeremy Faust. “There’s different levels of vaccination. There’s different levels of mitigation. And quite frankly, it’s a different time of year in South Africa.”
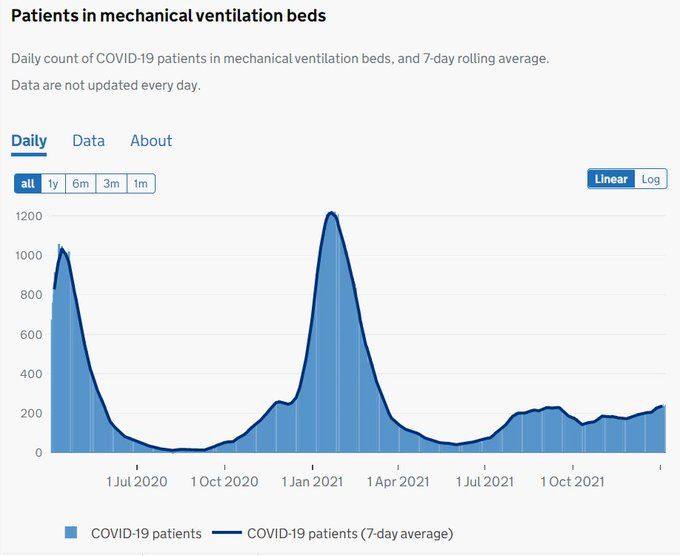
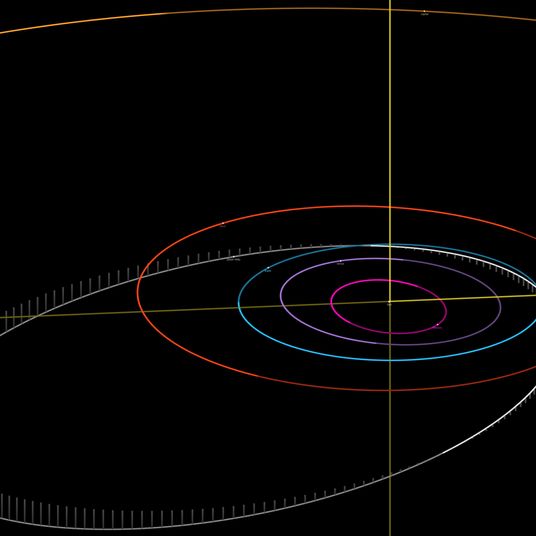
The data are already looking different, as well. Consider this chart from the U.K.’s NHS dashboard:
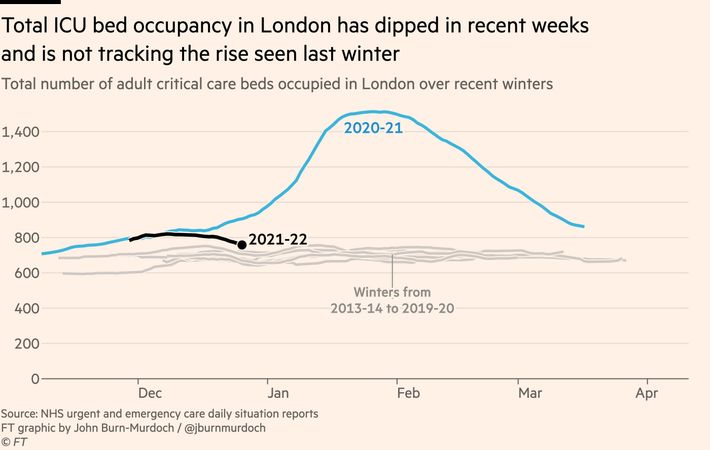
Total hospital admissions are indeed still rising in London, as are ICU admissions and the number of patients on ventilators. But the number of patients who have needed critical-care beds is bending well below the catastrophic NHS experience of last winter (as you can also see in these charts from John Burn-Murdoch and the Financial Times).
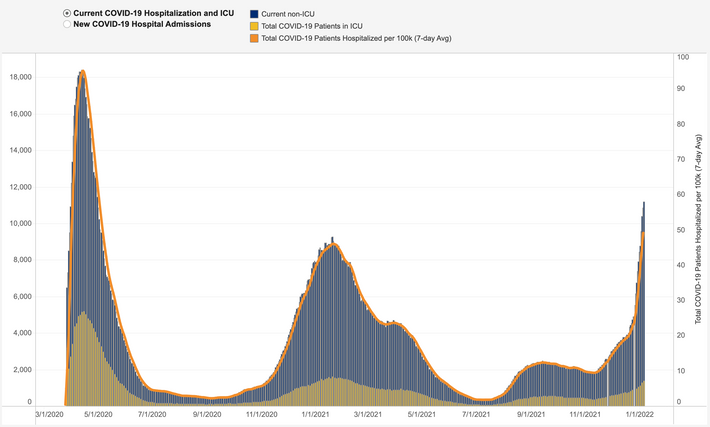
Now compare with the below chart, from the New York Department of Health, of statewide hospitalizations (in gray) and ICU admissions (in yellow). The spring 2020 peak is the first bump, the winter surge the second, and the Omicron wave coming ominously into view all the way at the right.
These charts aren’t exactly equivalent — one shows patients in need of ventilators and the other hospitalizations and ICU admissions. But comparing the ongoing Omicron spike on the right to the large winter wave in the middle, two things are very clear. The first is, in New York, both hospital and ICU admissions are obviously still on the rise, even if we are at or close to a local peak of cases. The second is, by both measures things are already nearing or past the heights of our previous wave. From here, Omicron is certain to trace a taller curve, at least, and perhaps a larger one, depending on how quickly the wave subsides. And for the moment, it is not looking much less severe at the population level than the intermediate surge last winter; in terms of total people in the hospital and ICU, it is looking likely to be at least as bad and potentially considerably worse.
In London, ICU demand is not just way down from last winter, it is already declining:
In New York, it is not just approaching last winter’s peak but clearly on the rise:
Of course, last winter was not New York’s worst period of the pandemic, as it was for much of the rest of the country (and England and much of Europe). New York’s worst phase came right at the start, in spring 2020, and though the next few weeks remain uncertain, it seems unlikely that the city or the state will reach the awful heights of that first wave, when more than 18,000 COVID patients were hospitalized, more than 5,000 of them eventually in ICUs.
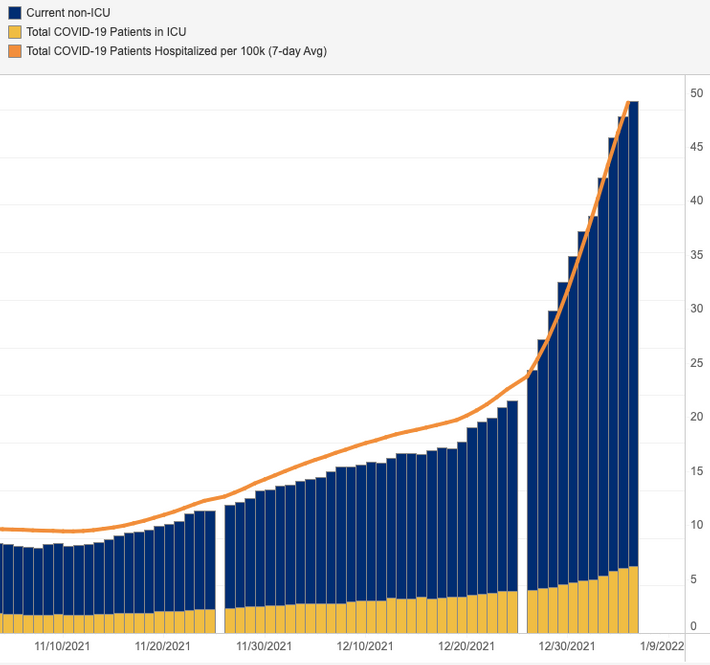
But a look at the country as a whole shows the same troubling pattern, as illustrated in this chart, by Burn-Murdoch and the FT:
There is a national decoupling, yes, in the sense that cases are shooting up much higher than hospital admissions and ICU patients. But each of those levels is already approaching the worst heights of the pandemic, and Omicron is just now starting to roll through the hospital system. Burn-Murdoch estimates that in “in wealthy, well-boosted countries like the U.K., deaths may peak at 10–15 percent of the previous record. In others, they may hit 50 percent.” Those are encouraging estimates, especially given how large the case growth has been. But the U.S. began the Omicron wave at close to 50 percent of its previous peak, and those lines on the right are all pointing pretty sharply up. The ultimate outcome is not yet clear, but if the early course of Omicron through Europe suggested a decoupling of cases from hospitalizations and deaths, the early course of the variant through the U.S. suggests a decoupling from that encouraging European path.
Why might our Omicron surge be different from the European one? Looking at the country as a whole, one big answer is obvious: Our vaccination rates are markedly lower than most European countries. (That is the hypothesis put forward by Burn-Murdoch, examining the divergent patterns of decoupling in the U.S. and U.K.) A second related answer is that we’ve done an even worse job, compared to our European peers, vaccinating and boosting the elderly. (Eric Topol of Scripps has emphasized this fact.) A third possibility is that the relatively high levels of severe disease we are seeing in New York and throughout the U.S. are the residue of that lingering Delta wave — either the effect of some limited amount of ongoing spread of the more virulent variant or the impact of cases that began their clinical cycle a few weeks ago and are still requiring treatment in the hospital. In some parts of Europe, like France, Omicron has been growing on top of Delta, but most of the continent and the U.K. had not been dealing with nearly as much severe disease this fall as the U.S. has been. This is Gounder’s hypothesis, echoed by other doctors and public-health officials who are advising caution in making any assessment of the American wave before Omicron truly takes over the hospitals — that we should wait for another week or two of data to see a clear picture of the new variant unclouded by the old one.
But we may already be past that transition, given that 95.7 percent of cases sequenced in New York between December 19 and January 2 were Omicron, and more than 18,000 New Yorkers have been hospitalized since December 26. And while the “lingering Delta” hypothesis might well explain some early-Omicron-observed severity at the national level, New York didn’t have a big Delta caseload in the late fall to begin with — by national standards at least.
On top of which, New York has a different vaccination profile than the country as a whole: 72 percent of New Yorkers have gotten at least two shots of vaccine, compared to 62 percent for the U.S. and 70 percent for the U.K. The Brits have done a considerably better at the critical job of delivering boosters — just over half their population has been boosted — but in terms of overall vaccination, New York State may be as close to the U.K. and other European countries as it is to the rest of the American states, where rates are often much lower. All this makes the concerning New York data potentially even more concerning, suggesting that outcomes here might not be representative of the American experience to come, but in fact milder, on the whole, than we will see in the rest of the country, assuming that Omicron cases soon overwhelm those places.
But one apparent difference between New York and Europe may also prove significant, if our Omicron wave continues to be more severe: Even though our vaccination rates may be comparable, we appear to be seeing a much bigger share of cases among the unvaccinated here than they have over there.
In fact, across Europe, wherever surveillance has been conducted, it has demonstrated that Omicron is spreading very proficiently among the vaccinated, which may be one reason why the overall severity of the surge looks so low (those people are much less protected against infection with the new variant, given its apparent immune-escape features, but especially if they are boosted they remain very well protected against severe disease caused by it). All of this data is better than the American equivalent, but it still has shortcomings and limitations: Some countries count two shots as fully vaccinated, some count three; some distinguish between the two groups, but some don’t; and none are sophisticated enough to carefully track the effect of immunological waning in their official reports. Nevertheless, taken altogether the picture European data gives is very clear, with the share of Omicron cases among each country’s vaccinated population equal to or greater than the vaccinated share of the population as a whole. In Germany, where 71 percent of the country is double-vaccinated, 78 percent of the country’s Omicron cases have been among the vaccinated, it was estimated. (A data error at first made it seem the share was even higher, but it has been corrected.) In Denmark, where 80 percent are, it is 81 percent. Because vaccination does protect so well against severe disease, in any particular place hospital admissions should skew much more dramatically toward the unvaccinated than do cases, and yet, in the U.K., more than two-thirds of their hospitalizations have been patients with two or more doses of vaccine.
That these shares are large is not so surprising, given what we know about Omicron’s immune-evasion properties. And as we’ve heard again and again since the rollout of vaccines, as the vaccination level of a population grows, so too will the share among the vaccinated of new cases (and even, ultimately, severe cases). But the fact that the share of cases among the vaccinated so closely matches the share of the population that is vaccinated suggests that, in Europe, though the seriously ill are more likely to be unvaccinated, in terms of pure caseloads, Omicron has been spreading about equally through vaccinated and unvaccinated populations.
This pattern is not what we are seeing in New York, where, according to the state, the unvaccinated were — at the end of December, after Omicron took over — eight times more likely to be diagnosed officially than were the vaccinated. Presenting this data alongside the European numbers does not make for a perfect comparison, since one is a raw accounting of spread and another a population-adjusted calculation of risk, and since neither accounts for the age stratification of vaccination, which is crucially important. But pandemic comparisons are never neat, especially this early in a wave, with so much noise in the data, and the contrast is striking nevertheless. And given how much more well protected the vaccinated are against severe disease, with Omicron as with every other variant, even a small difference in the share of spread among the unvaccinated could make the overall picture look significantly more severe. According to Gounder, two thirds of the patients newly hospitalized at Bellevue, where she has recently been on service, are completely unvaccinated — a reversal of the British data. And the data from elsewhere in the country is similar: 80 percent of hospital admissions in Louisiana were not fully vaccinated, and 71 percent in Connecticut.
The reasons for this apparent pattern are not obviously clear, though it may reflect some amount of statistical noise; the particular subpopulations through which the variant happened to get an early foothold; the relatively larger number of unvaccinated Americans; or social dynamics beyond our intuitive grasp or modeling capability. If the pattern holds, though, it could prove a grim sign.
To this point, however, reporting from inside American hospitals has been relatively reassuring — doctors have tended to describe less pressure on ICUs and, overall, a picture of less severe disease than has been observed at previous points in the pandemic. Doctors have also emphasized how many patients have been hospitalized “with” COVID, rather than “for” COVID. Indeed for the first time today New York State has begun, at the direction of Governor Hochul, distinguishing between those patients whose COVID is “incidental” to their hospitalization and those who were admitted expressly for the disease. In the first day’s data, 41 percent of COVID admissions in New York were incidental, and in many hospitals across the country, the number of patients admitted with incidental COVID outnumber those admitted for COVID treatment; in Los Angeles, among recent admissions, it’s been two-thirds. And in New York, 37 percent of those recently diagnosed at the hospital are asymptomatic.
But while Gounder says there are “absolutely” more patients with “incidental” COVID during this wave, the two are not precisely defined categories. Faust has emphasized a third group — those who have other medical issues but have been “tipped over” into hospitalization by the presence of COVID. To me, he also mentions a fourth group — the “hospital onset” cases, where patients admitted for another issue catch COVID while hospitalized. For some of them, the new infection could be not trivial but a catastrophic complication, and, Faust says, hospital onset cases are now at record highs for the pandemic — among the worrying signs he’s watching at the moment.
“I think that so far we have experienced what I would call a buffer between this massive rise in cases and the effect that has had on the hospitals” — the wave has not yet fully worked its way into the hospital systems, in other words. “That’s for a lot of reasons,” Faust says. “That’s due to population immunity. That’s due to maybe Omicron being a bit milder — I think that’s real. And in many places, it’s a result of a younger, healthier population being the ones driving the outbreaks at first.” This makes it hard to project early data on severity out through the end of a given wave, since the sorts of people sick now with Omicron aren’t necessarily representative. “It’s essentially the same thing as, as saying, if a vaccinated college has an outbreak and an unvaccinated nursing home has an outbreak, those produce two very different pictures,” Faust says. “20,000 sick college kids can have less of an effect on a hospital than 200 sick nursing-home patients.”
A few weeks ago, Faust helped launch a hospital-capacity dashboard with Bill Hanage and Benjy Renton. At the moment, it shows that eight states, including California and Texas, have reached a circuit-breaker level — meaning that additional mitigation measures are needed to preserve proper ongoing hospital functioning. Thirteen more, including New York and Florida, are now operating at an “unsustainable” level.
“What’s happened in the past few days is that threshold — how many cases we could tolerate before hospitals really feel it — has been leapfrogged by the cases,” Faust says. “So that’s where I’m getting worried. On top of that, the relative mildness of this disease has also made it so that ICUs have lagged, as well. And what gives me great concern is that in the past week or so, around the country, you started to see outbreaks in nursing homes. That was not happening before,” he says. “When I look at the data that I’m looking at, there’s a range of possibilities that could be absolutely catastrophic. And I can’t rule ’em out yet. And that’s why I’m sitting here sort of nervous.”
What worries Faust most is what he calls “the sort of zombie-apocalypse scenario, where you truly have to pull patients off of ventilators and not have enough oxygen.” This was what famously happened early in 2020 in Italian hospitals and became the source of the largely successful “flatten the curve” rallying cry for Americans later that spring. “There was almost no place in the country that had to really use crisis standards of care,” Faust says. “We didn’t stomp out the virus, but we certainly didn’t get in a situation where there were 35 patients in an ICU but only ten ventilators, and so 25 of them were just dying.” And now? “There’s a great portion of the country right now that is at risk of entering into that kind of situation sometime soon,” he says. “Will that happen? I don’t know, but I always prefer when I can say, I don’t think that will happen.”
More About the Omicron Wave
- What to Know About the New COVID Booster Shots
- The Dismantling of Hong Kong
- What We Know About All the Omicron Subvariants, Including BA.2.12.1