It’s always dangerous, in a fast-moving pandemic, to take a freeze-frame of the present tense and trust that you can see the future in it all that clearly. In the last few days, there has been a wave of good news about Omicron: Cases appear to have peaked in New York and Boston, possibly D.C., and even perhaps the country as a whole. Given the rapid rise and fall of waves elsewhere in the world, this is not too much of a surprise, and most experts expect the descent from the peak to be roughly as steep as the ascent, which means we may be in a much, much better place, infection-wise, in just a few weeks. But the incredibly fast spread of Omicron also means that by other important metrics — hospitalization and death, in certain obvious ways the most important metrics — the worst is still almost certainly ahead of us. Conceivably, by those measures, things could get a lot worse before it gets better.
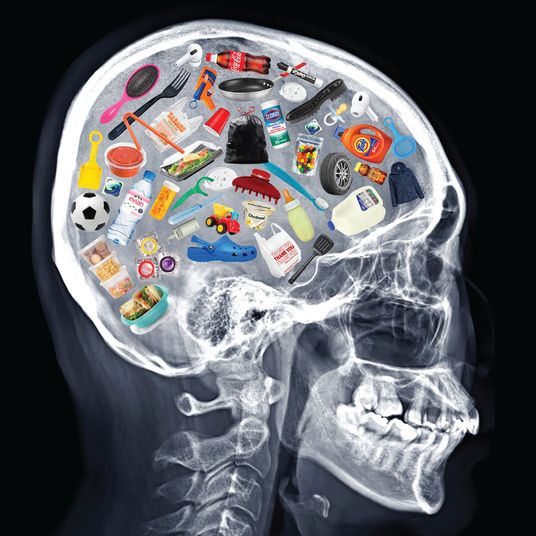
Over the last few weeks — as Omicron first announced itself, in South Africa, and then revealed itself, there and in Europe, as a relatively mild if remarkably transmissible variant — there has been a growing rumble of proposals to move away from the spread-based metrics the country has relied on throughout the pandemic, namely cases, toward one that measured severe outcomes instead, namely hospitalizations. This advice has come not just from those who’ve long advised we panic a little bit less about the virus, like Monica Gandhi, a professor of medicine at the University of California, San Francisco, but also establishment voices of the liberal center, long on the other end of the panic spectrum, like Anthony Fauci and the New York Times. There may well be some wisdom in this shift, in the long term — perhaps even as soon as the other side of this Omicron wave, when the hospitalization data may start to look much more encouraging. But the timing has been almost comically poor because, in the short term, that new metric doesn’t tell an encouraging story at all. Hospitalizations in the country are at a record high, meaning that more Americans are now being treated for serious COVID than at any point in the pandemic. That includes the first wave, with its images of mobile morgues and hospital ships and patients waiting in ambulances outside emergency rooms; it includes the winter surge, which unfolded before mass vaccination and has been, to this point, the deadliest phase; and it includes the Delta wave, when vaccinated Americans who began tuning out the bad news from the rest of the country may not have noticed that 200,000 of their fellow citizens died this past fall.
The vaccinated and boosted remain well protected against severe outcomes, but to use that preferred metric of those urging a conceptual phase shift toward “living with the virus” — hospitalizations — the country as a whole is not in a better place at all. Indeed, to use that metric, we are in the absolute worst spot the country has been in at any point over the last two years, during which time more than 800,000 Americans have died. We are already living with the virus; it is also hospitalizing us in unprecedented numbers.
Of course, the story is a bit more complicated than that. We can already see that this wave, however brutal, is almost certain to pass quickly. Many of those hospitalized are experiencing only “incidental” COVID — hospitalized for other reasons and diagnosed only after they were admitted. (Depending on the hospital system, estimates of this share of admissions range from about one-third to about two-thirds.) But ICU admissions are a bit less squishy, and while the Omicron wave hasn’t yet set a record there, it has already brought the total number of ICU patients past 25,000; the peak last winter was just above 28,000, and the numbers have been growing, lately, at about a thousand per day.
On Tuesday, a large, preprint study from Southern California painted what counts as an encouraging picture: a 50 percent lower hospitalization rate with Omicron than with Delta, a 75 percent lower rate of admission to the ICU, and a 90 percent reduction in mortality. These reductions are in line with what has been observed in Europe, where Omicron has produced some serious illness and death but dramatically less than might’ve been predicted given the case numbers. If they hold for the country as a whole, it would mean that early indications the American Omicron wave would be more severe than experienced across the Atlantic were false or misleading signals, and that the wave here would be — while intense — somewhat less brutal overall than previous ones.
But, worryingly, at the moment there is data pointing in the other direction as well. On Sunday, the Times published an eye-opening group of charts to illustrate the early shape of American mortality during the Omicron surge. Compiling data from New York City, Chicago, and Boston, what they found was — given everything we know about immunity and about Omicron — almost hard to believe. In each case, shifting the graphs by 21 days to account for the typical lag between diagnosis and death showed that the number of deaths was now growing almost precisely in line with case growth. In other words, in this data at least, there was been almost no “decoupling” between cases and deaths at all — to this point, in these places, the Omicron wave appeared on a per-case basis just about as deadly as last winter’s surge, when hardly anyone in the country was vaccinated and the virus itself was inherently more virulent than this variant. In South Africa’s Omicron surge, there was a 30-fold reduction in case-fatality ratio from their previous wave — a decline of more than 95 percent. In Europe, the decoupling hasn’t been quite as dramatic, but in country after country, the divergence in cases and deaths is striking nevertheless. This set of American data suggested declines of just 10 or 20 percent.
When you have as many cases as we do now, that isn’t just a recipe for a rougher wave than has washed over Europe. It’s a recipe for something much more catastrophic. If this pattern — rather than the one observed in Southern California — holds true for the country as a whole, it would mean that even without much additional spread from this point, the national death toll could rise well past the previous pandemic peak of just over 3,000 deaths per day from last January to 5,000 or even 7,500 deaths a day. Possibly more. Yesterday, 2,665 American deaths were reported, and the number is rising.
That peak won’t last long, since even if we are not replicating the reductions in severity observed in South Africa and Europe, we do seem to be replicating the compressed shape of their waves, mercifully. But even with such a fast peak and decline, the patterns observed in New York, Chicago, and Boston suggest that, nationally, the end result could be 100,000 Americans dead in a single month from a variant a lot of people have spent a lot of time the last few weeks describing as “mild.”
Is this alarmism? Let’s hope so, which is to say, let’s hope that the national Omicron wave looks a lot more like the data we have from Southern California than from New York. And there are some good reasons to think it might — or at least to be cautious in extrapolating that New York data too confidently.
First, the Times case study is small — just three cities and not necessarily representative ones. On the other hand, they are places with relatively high vaccination rates and levels of previous infection, both of which, in theory, make them less vulnerable to severe illness than the rest of the country, not more.
Second, there is a possible calendar complication. Because the observed cases are from December 21 in the Times data, it is possible that some portion of the deaths that followed reflect cases of Delta rather than Omicron. On the other hand, none of these cities were dealing with especially brutal Delta waves earlier in the fall, and we know that between December 19 and January 2, 95.7 percent of cases sequenced in New York were already Omicron. The next week or so will help illuminate the distinction since deaths recorded a week or ten days from now will be almost certainly cases of Omicron. In the meantime, since the Times reported its data, New York State deaths have climbed from 86, on January 8, to 266, on January 11. Day-to-day is noisy, of course, but the smoothed seven-day average marks a clear upward trend too — from a daily average of 120 to a daily average of 156 in just three days.
There is also the fact that the generational time of Omicron — which appears considerably shorter — may complicate any effort to apply a simple 21-day lag; if the lag between cases and deaths is smaller, a 21-day comparison would overstate the mortality rate by connecting a relatively later (and higher) death figure to an earlier (and lower) case figure. (This is a danger of analyzing case numbers that are changing so quickly — choosing the wrong start date by just two or three days could mean messing up the math by as much as a factor of two.) And there is encouraging data on this point from the big Southern California study, which showed a reduction of 69 percent in the length of hospital stays with Omicron, suggesting a shorter duration of illness and implying a shorter lag. This would mean that, in New York City, deaths on January 8 did not reflect cases diagnosed on December 21 but potentially cases at least several days later, and maybe more, shifting the curves enough that the Omicron wave was no longer tracking the course of the winter surge but instead tracking significantly below. On the other hand, in South Africa, cases appear to have peaked around December 17, and deaths have not yet peaked, more than three weeks later — suggesting that, at least in South Africa, the appropriate lag to apply for Omicron might be longer than 21 days, not shorter.
Testing issues and the incompleteness of our picture of Omicron spread may also scramble the analysis, since we may be missing a larger share of infections with this wave than previous ones. On the other hand, the country is now testing more than it has at any point in the pandemic, and even if it was the case that more cases were still being overlooked, that would only change our picture of the relative mildness of this wave, not the scale of its impact. In other words, if the true number of new daily infections was 7.5 million rather than 750,000, it might make a projected death toll of 7,500 daily deaths several weeks from now seem relatively smaller — but it wouldn’t actually reduce the number of projected deaths.
While the experience of Omicron in South Africa and across Europe should give Americans some comfort, even the question of how much milder the Omicron variant actually was there is complicated and uncertain. In a preprint study, researchers found only a 25 percent reduction in inherent severity compared to Delta (the country’s growing “immune wall” explaining the rest of the decrease). That estimate may be revised in future studies, including those looking at Europe and the U.S., but at the moment, it is an eerily close match for the Times data. A 20 or 25 percent reduction isn’t insignificant, of course; but we already have four times as many cases today as we had at the Delta peak. If you multiply Delta fatalities by four and then reduce them by 25 percent, you do not get a pretty picture. You get a death peak — even a very brief one — three times as high.
Will that come to pass? Everything we’ve seen abroad suggests it shouldn’t, and reporting from within American hospitals continues to emphasize, even as they find themselves overwhelmed with patients, the relative mildness of illness with Omicron. But what makes the darker path more plausible than it might seem at first blush is the American experience of Delta. Then, too, we watched early data from the U.K. and were encouraged — only to see the American trajectory depart pretty radically from the baseline expectation formed by the European experience. And if what changed between Delta and Omicron in South Africa was primarily a change in population-level immunity (through some vaccination and a lot of infection), the picture we have of national immunity here is more or less unchanged since Delta. That wave produced substantial infection-derived immunity, of course, which does expand population-level defense against future illness and death. But the vaccination rate hasn’t changed much since Delta, and indeed the effect of waning and the slow uptake of boosters suggest, at least on the vaccination side, the country may be now less well protected against Omicron than the previous variants. Which makes it all the more notable that in England, overall population-level severity appears to have declined much more before Delta, as a result of vaccination, than with Omicron, as a result of reduced virulence. In other words, the “decoupling” between cases and deaths we are pointing to in the U.K. — and which has given so many Americans an optimistic read of this surge — occurred primarily during the Delta wave. The divergence has been larger with Omicron, but not dramatically so.
Consider the following numbers. At its Delta peak, the U.K. was recording an average of about 130 deaths per day, following from a case peak of around 47,000; with Omicron, the death total still hasn’t peaked but has reached an average of about 240, following a case peak of about 180,000. About a four-fold increase in cases has produced, so far, about a doubling in deaths, which are still rising. Even if we assume that U.K. deaths are now at their peak, those numbers would imply a rough halving of the case-fatality ratio with Omicron — a meaningful reduction but not a game-changing one. The far more dramatic difference is between the Delta wave and the previous winter peak, when 60,000 daily cases produced about 1,200 daily deaths. In the U.K., between that point and Delta, a tripling of daily cases produced one-tenth as many deaths. That is a 30-fold reduction, an effect 15 times the change observed with Omicron.
And if it is those reductions — before Delta, from vaccination — that have landed the U.K. and indeed much of Europe in a much better place now, it is concerning that we saw nothing like them, over the same time period, here in the U.S. Here, there was essentially no change at all in the ratio of cases to deaths between the pre-vaccine winter surge and the post-vaccine Delta wave. Last January, a case peak of 250,000 produced, ultimately, a death peak of about 3,400; with Delta, a case peak of about 160,000 produced a death peak of about 2,100. Just under two-thirds as many cases produced just under two-thirds as many deaths. It was as though, in the interim, the vaccination rollout hadn’t happened at all. Of course, we know that vaccines do work — study after study about the divergent outcomes of the vaccinated and unvaccinated show an enormous effect. But at the national level, the effect of mass vaccination was weirdly invisible, at least with Delta — the vaccines and that variant roughly fighting to a draw. In Europe, they observed the predicted effect of mass vaccination; here, with only somewhat lower rates, there was hardly any effect at all.
Exactly why this happened remains a bit of a mystery — indeed, to my mind, it is one of the great mysteries of the whole pandemic. But it also raises an uncomfortable question about the Omicron endgame: Will our fatality numbers more closely track those of European countries or of our own recent past? Will Omicron render Delta an anomaly and tragic curiosity of the pandemic, or will it prove to be another episode in which, for a variety of reasons — some known, like lower vaccination and booster rates, and some still unknown — America performs much worse than the early international data on which we based our expectations implied we should?
Whatever happens, it seems certain the wave will be fast, which means both that we will know the answer quite soon and that, when we do hit the mortality peak for Omicron, whether it is 3,000 deaths per day or 6,000, we may be already so far down the roller coaster of cases and so excited — the “vaxxed and done,” especially — to exit this phase and move on that we hardly even note the highest number of new deaths the country recorded on any day through the whole pandemic. Relief from Omicron is coming, inevitably and soon. But there’s a pretty good chance that — two years on, with more than 500 million vaccine doses administered — that day of record death is still ahead of us.
More on Omicron
- What to Know About the New COVID Booster Shots
- The Dismantling of Hong Kong
- What We Know About All the Omicron Subvariants, Including BA.2.12.1