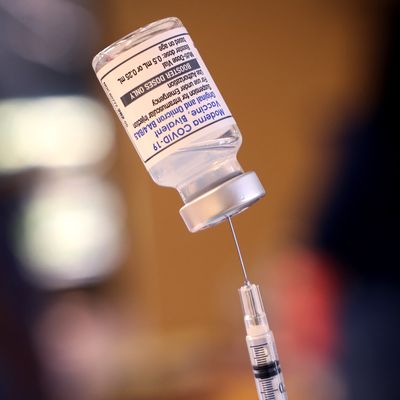
At the beginning of September, the FDA authorized bivalent COVID booster shots from Pfizer and Moderna that have been reformulated to target both the original strain of the coronavirus and the lineage of the Omicron variant, including BA.4 and BA.5, which continue to make up nearly all new cases in the U.S. The CDC has recommended that everyone 12 and over receive the updated formula whenever they are next eligible for a booster, and countless Americans have been getting the shots as the new boosters continue to become more widely available across the country. As COVID continues to spread at high levels throughout the U.S., the Biden administration is heavily promoting the bivalent boosters, hoping to limit what has traditionally been a fall and winter COVID surge as people begin to spend more time indoors. The effort also comes at a time when only about a third of Americans 50 and over have gotten, as recommended, their second booster shot. The administration has even announced that most people could only need an annual COVID booster from now on, similar to the annual influenza vaccine. Below is a look at some of the most important questions, controversy, and criticism about the updated boosters and the rollout thus far.
Have these new boosters been tested enough, and do they actually work better?
There has been some controversy surrounding the way the updated boosters were tested and approved in the U.S., but that doesn’t mean they aren’t safe or won’t work — but how well they work remains to be seen.
The U.S. isn’t the only country rolling out bivalent COVID boosters, but it has taken a different approach — and that has led to some pushback from infectious-disease experts, as well as reformulated attempts to discredit the new shots by anti-vaxxers.
Other governments, like in Canada and Europe, have thus far only approved bivalent boosters that were reformulated to target the original Omicron strain, BA.1, and have undergone human trials. The U.S. had the opportunity to do the same, but instead requested that the pharmaceutical companies develop — and prepurchased — further updated boosters that also target the newer BA.4 and BA.5 variants. Pfizer and Moderna did that, and the FDA and CDC then signed off on making the updated boosters available to the public without first conducting human trials.
That doesn’t mean the updated vaccines are less safe than their predecessors; these formulas are just slightly tweaked versions of the BA.1 reformulations that human trials showed were just as safe as the original COVID vaccines. That fundamental safety is extremely unlikely to have changed because of those tweaks. But what it does mean is that there isn’t yet evidence from human trials that the BA.4/5-reformulated vaccines are actually better than their predecessors. Everyone is just assuming they will do at least as good a job as the BA.1 reformulations at providing more protection against current COVID strains, and most likely do a better job. And while there is some limited preclinical data indicating they’ll do that better job, it is from tests using mice instead of people. The human-trial data is expected later this year, and as many COVID experts have been pointing out, the annual flu-vaccine reformulations are primarily tested on animals, as well.
The lack of human trials — and the whole mice thing — have, not surprisingly, been catnip for vaccine skeptics. Some infectious-disease experts have criticized the U.S. for proceeding in a way that might encourage vaccine hesitancy and potentially turn off would-be booster recipients at a time when the U.S. is already well behind other wealthy countries.
But there is also a matter of precedent and basic best-practice science, as infectious-disease doctor Céline Gounder and Kaiser Health News editor-in-chief Elisabeth Rosenthal explained in a recent op-ed:
The updated shots easily clear the “safe and effective” bar for government authorization. But in the real world, are the omicron-specific vaccines significantly more protective — and in what ways — than the original covid vaccines so many have already taken? If so, who would benefit most from the new shots? Since the federal government is purchasing these new vaccines — and many of the original, already purchased vaccines may never find their way into taxpayers’ arms — is the $3.2 billion price tag worth the unclear benefit? Especially when these funds had to be pulled from other covid response efforts, like testing and treatment.
They point out that the data from the clinical trials of Pfizer and Moderna’s BA.1-targeting formulas indicated they only offered a slight improvement in producing more neutralizing antibody titers than the original formulas. Others, like Children’s Hospital of Philadelphia doctor Paul Offit (who is one of two people on the FDA’s panel of expert advisers and voted against authorizing the BA.4/5 bivalent vaccine yet), want to confirm that the bivalent vaccine isn’t less effective than the original formula. And it also remains unclear just how much of a benefit any booster shot provides people under the age of 65 who aren’t immunocompromised.
Fast-tracking the BA.4/5-targeting boosters, Gounder and Rosenthal argue, also “leaves front-line health-care providers in the impossible position of trying to advise individual patients whether and when to take the hot, new vaccines without complete data and in the face of marketing hype.” And that hype is the other fire they worry the move will fuel:
As society moves into the next phase of the pandemic, the pharmaceutical industry may be moving into more familiar territory: developing products that may be a smidgen better than what came before, selling — sometimes overselling — their increased effectiveness in the absence of adequate controlled studies or published data, advertising them as desirable for all when only some stand to benefit significantly, and in all likelihood raising the price later.
Are we really ready to shift to an annual COVID booster?
“Barring any new variant curveballs,” White House COVID-response coordinator Ashish Jha announced on September 6, “for a large majority of Americans, we are moving to a point where a single, annual COVID shot should provide a high degree of protection against serious illness all year.” The Biden administration wants the timing of the annual shot to line up, like the annual flu shot, in September and October. And like the influenza vaccine, the COVID booster would be updated annually to address whatever dominant strains are in circulation. Seniors and others at higher risk of severe COVID may still need to get more frequent boosters, Jha said, but everyone else may be able to shift to this new predictable routine.
The problem with this plan, a variety of public-health experts have noted, is that the behavior of the coronavirus, up to this point, has been anything but predictable. It has undergone several dramatic mutations that have made it a formidable adversary for the human immune system, including for people who are vaccinated or have had previous infections. Though we’ve been able to build up a resilient wall of immunity that has made severe COVID rarer and rarer, the “variant curveball” scenario has thus far been a norm, not an outlier. And there are other potential issues, as The Atlantic’s Jacob Stern recently reported:
For one thing, it assumes that the virus will follow an annual schedule with peaks in the fall and winter — not unlikely, but also not a given. For another, we still don’t have a firm grasp on the magnitude or duration of the benefits offered by the new Omicron-specific vaccine. For all we know, [University of Pittsburgh School of Medicine professor Walid] Gellad told me, the added protection afforded to someone who gets the shot tomorrow may have largely dissipated by New Year’s Eve.
Stern also notes that there is some enthusiasm about the plan, since it would hopefully simplify what has been perpetually maddening and confusing public-health messaging about booster shots. On the other hand, as Gellad also pointed out, when have attempts to simplify COVID information ever gone well?
Is it about to be more expensive to get booster shots, and possibly more difficult?
Yes, it most likely will for a lot of Americans, because the Biden administration is currently planning to stop offering free COVID vaccines and treatments next year, citing the lack of additional pandemic funding from Congress (though it was always inevitable such a shift would eventually happen). This means preventing and treating COVID will soon be relegated to America’s famously expensive and complicated health-care industry and all its built-in inequities. Private health insurers and pharmaceutical companies will thus be given far more control over coverage and pricing, which will undoubtedly lead to higher premiums and costs for health-care consumers as these industries gain freer rein to boost their pandemic profit margins. As Céline Gounder and Elisabeth Rosenthal noted in their KHN op-ed:
The federal government has been paying a negotiated price of $15 to $19.50 a dose of mRNA vaccine under a purchasing agreement signed during the height of the pandemic. When those government agreements lapse, analysts expect the price to triple or quadruple, and perhaps even more for updated yearly COVID boosters, which Moderna’s CEO said would evolve “like an iPhone.”
And beyond higher costs for consumers, there are several other important factors that could prove problematic, including ensuring continued access to COVID vaccines and treatments for the uninsured, lining up some aspects of COVID care under Medicare and Medicaid, and making sure the U.S. has a large enough supply of vaccines and treatments to deal with future surges when the government isn’t paying to stockpile them. The pandemic isn’t over, after all, but Americans’ free access to pandemic-related health care soon will be. The next few months will likely be the last opportunity to get vaccinated and boosted on the government’s dime.
What about getting a COVID booster and a flu shot at the same time? Is that a good idea?
The Biden administration is also now encouraging people to get flu shots along with their COVID boosters. “I really believe this is why God gave us two arms — one for the flu shot and the other one for the COVID shot,” Jha recently remarked. It’s safe to get both shots at the same time, and there are some indications that the upcoming flu season may be the first bad one the U.S. has experienced since before the COVID pandemic, so it makes sense that the government is advising people to get both shots at once. But the idea has also received some pushback from infectious-disease experts. Their concern, as Stat News recently reported, is that the protection a flu shot provides is short-lived — typically lasting about four months — which could leave early shot-getters exposed if the coming flu season doesn’t peak until late winter like it did last year. “I understand why this is promoted,” flu expert Florian Krammer told Stat, “but from an immunological point of view, it doesn’t make much sense.” He’s going to wait until November to get his flu shot, while other experts suggested late October. Others acknowledged that getting flu shots into more arms, which is always a perennial challenge, may be worth the timing trade-off.
So it seems that the best guidance is that for people who are definitely going to get a flu shot no matter what, they should hold off until late October if they are willing and able to do that — unless directed otherwise by their doctor. At the same time, timing isn’t everything, particularly since nobody knows when, in fact, this flu season will actually peak.
Which new booster is better?
While it’s certainly possible one of the new bivalent boosters will perform marginally better than the other, there isn’t data to determine that yet. For now, it’s likely that the both the Moderna and Pfizer shots will be comparable, just like their original formula vaccines were.
How well will these new boosters protect against future variants?
One of the most substantive criticisms of America’s booster strategy is that targeting the Omicron lineage, as well as future boosters targeting other lineages if and when they appear, may not be as effective as investing in next-generation COVID vaccines that could be futureproof and/or more effective at preventing infection in the first place. Such vaccines, including intranasal and universal coronavirus vaccines, are currently in development, but at nothing like the scope and speed of how the first COVID vaccines were developed during the highly effective, extremely well-funded Operation Warp Speed.
And it remains possible that a new COVID variant will soon arrive that has made some evolutionary leap that renders existing vaccines, including the new bivalent ones, much less effective. If and when that happens, both the U.S. and the manufacturers of the bivalent vaccines could be stuck playing, as Scripps’ Eric Topol has described it, variant Whac-a-Mole. But for now, at least, that Variant X is not yet on the horizon. At present, the Omicron lineage makes up everything on the board. BA.5 still accounts for nearly all COVID cases in the U.S., followed by BA.4.6 — which appears to be able to outcompete BA.5 and is gradually making up a larger fraction of U.S. cases, but does not appear to represent a unique new threat. Most likely, the new bivalent boosters will be effective — and probably more effective to some degree — against this lineage. And nobody should be holding out for something better to become available. If you’re eligible for a booster, go ahead and get one.
This post has been updated.