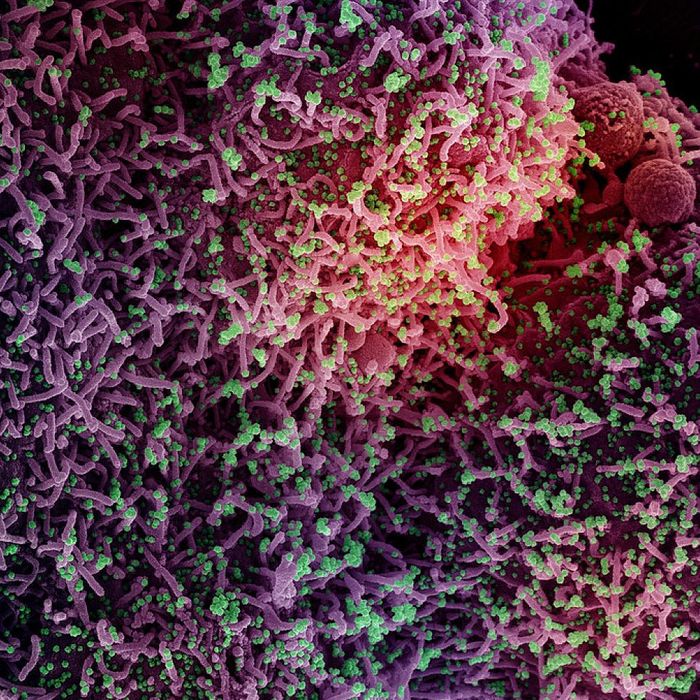
After many months of global dominance by the Omicron subvariant BA.5, an alphabet soup of newer Omicron strains is now rising in the U.S. and abroad as SARS-CoV-2 continues to rapidly evolve. Though BA.5 still accounts for more than 60 percent of new U.S. COVID cases, that percentage has been steadily dropping for weeks. But unlike past progressions of variant competition and dominance in the country and world, there isn’t one single variant that has been supplanting BA.5 but multiple independent strains in the Omicron lineage with similar mutations rising in different places around the world simultaneously. In the U.S., there are now five subvariants rising over the past few weeks. As one biosecurity researcher recently commented on Twitter, “Welcome to the Omicron Olympics.”
Most COVID experts seem to agree that one or a combination of these variants will inevitably trigger another wave, or multiple waves, of U.S. cases over the coming months, though how big remains difficult to predict. New variants are not the only factor that drives up new cases: The abandonment of public and personal precautions, waning immunity, and seasonal patterns, like people spending more time indoors when it’s cold, play a role as well. There are also concerns that some of the monoclonal antibody treatments currently used against COVID will be less effective or fully ineffective against some of the new strains. It is, in other words, another new and confusing phase of the pandemic. Below, what we know about the rising subvariants, including BQ.1 and BQ.1.1, BF.7, BA.4.6, and XBB
How are all of these subvariants different from their predecessors?
Most of the rising subvariants around the world (about 75 percent) are descendants of BA.5. The most notable half-dozen or so new strains have all shown some degree of growth advantage over BA.5 and other predecessors, which means they have likely evolved to be more transmissible and immune evasive to varying degrees.
There does not appear any evidence that any of them are more virulent than previous strains, however.
What is also notable about these strains is that they demonstrate what is called convergent evolution; they share similar mutations — despite being distinct strains — as a result of facing the same wall of immunity in humans. For instance, four of the most prominent new strains (BA.4.6, BF.7, BQ.1.1, and BA.2.75.2) share the same R346T spike protein mutation, which has been linked to greater immune evasion.
But the biggest concern about this new group of subvariants is that many of them appear resistant to existing monoclonal antibody drugs. Five — BA.2.75.2, BA.4.6, BF.7, BQ.1.1., and XBB — have been shown in studies to be resistant to Evusheld, which has been one of the most important protections against COVID for people who are immunocompromised. Two — XBB and BQ.1.1 — have been shown to be resistant to the monoclonal antibody drug Bebtelovimab as well.
What’s with all the confusing letter names?
While the WHO has used Greek letters to identify the major COVID variants in the past, global public-health authorities have not come up with a new system of identifying Omicron subvariants, which currently make up the entire landscape of COVID strains circulating in the world. That leaves the more technical alphanumeric-based names, some of which are used to aggregate what are effectively sub-subvariants. Though some scientists have started dubbing some of the prominent Omicron subvariants with unique names (Cerberus, Typhon, Aeterna, Gryphon, etc.) — those monikers have not become commonplace, have not been used by public-health authorities, and are probably just adding to the confusion.
Which new subvariant is the most worrisome, overall?
Some of the new strains have been individually described as the most immune-evasive variants seen yet based on early research indicating one or the other is better equipped than its predecessors at getting around antibodies produced by prior infection, vaccination, and monoclonal antibody drugs. Such superlatives are confusing, however, when they are being used to describe multiple variants more or less at the same time. It’s not yet possible to determine which of these variants is comparatively the most transmissible or most immune evasive, and there’s no evidence that they cause more serious illness. All that being said, the two variants drawing the most attention from scientists right now are the BQ.1 and XBB lineages.
How well do the vaccines and new bivalent boosters work against these new strains?
While there may be some drop off in vaccine effectiveness against any new COVID strain that has evolved to get around our wall of immunity, it will be a matter of how much and for whom, depending on a range of factors, including how up-to-date someone is on their vaccinations.
Will the new bivalent booster shots available in the U.S. — which were reformulated to specifically target the BA.4 and BA.5 subvariants — be effective or more effective against these new strains? Probably, since most of the new variants are in the BA.4 and BA.5 lineage. How much more effective remains to be seen.
The New Variants Scientists Are Watching
BQ.1 and BQ.1.1
This pair in the BA.5 sublineage is now drawing a lot of attention in the U.S. on account of how quickly the two variants have been rising. As of the week ending October 22, the CDC estimates that the pair made up a combined 16.6 percent of new U.S. cases, up from a combined 11.4 percent the previous week and 5.7 percent the week before that.
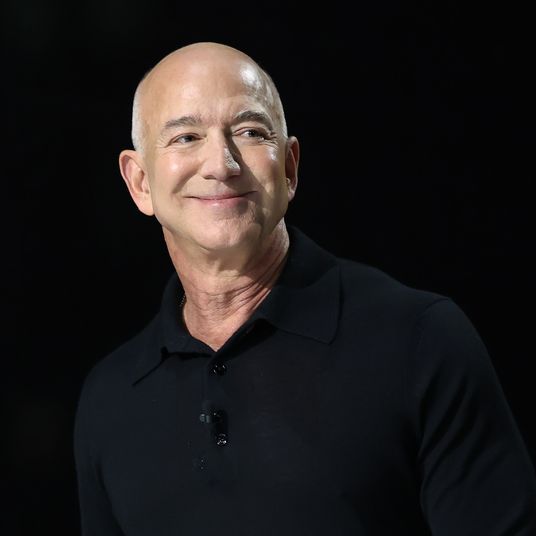
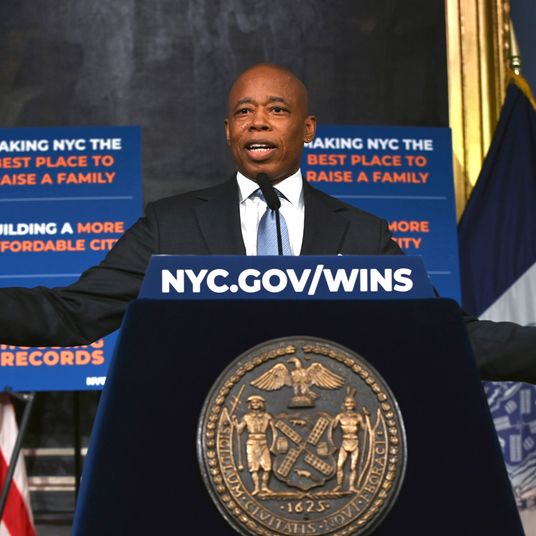
BQ.1 and BQ.1.1 appear to be rising fastest in New York and New Jersey, where they made up more than 28 percent of new infections as of the week ending October 22.
There isn’t enough data regarding the severity of the illness caused by these subvariants to draw firm conclusions, but no one seems to be sounding any alarm bells about their virulence yet.
BF.7
As of the week ending October 22, this descendant of BA.5 made up a CDC-estimated 6.7 percent of cases in the U.S., up from 5.3 percent the previous week. Like the others, BF.7 is believed to be more immune evasive than BA.5.
BA.4.6
This subvariant has two additional spike protein mutations differentiating it from its BA.4 parent. BA.4.6 has remained the second-most-prevalent strain in the U.S. for many weeks, and while its share of cases has increased over that time, its growth nationally has not been dramatic. As of the week ending October 22, the CDC estimated that BA.4.6 accounted for a little more than 11 percent of new U.S. cases, after hovering around 12 percent for a few weeks.
Some early research suggests BA.4.6 is better equipped than BA.5 to escape neutralizing antibodies by prior infection or vaccination.
BA.2.75 and BA.2.75.2
This subvariant lineage first raised alarm abroad over the summer for its potential immune evasiveness, according to early research. The two variants have been rising slowly in the U.S. but have yet to gain much of a hold. As of the week ending October 22, BA.2.75.2 made up 1.3 percent of cases and BA.2.75 made up 1.6 percent, according to CDC estimates.
XBB
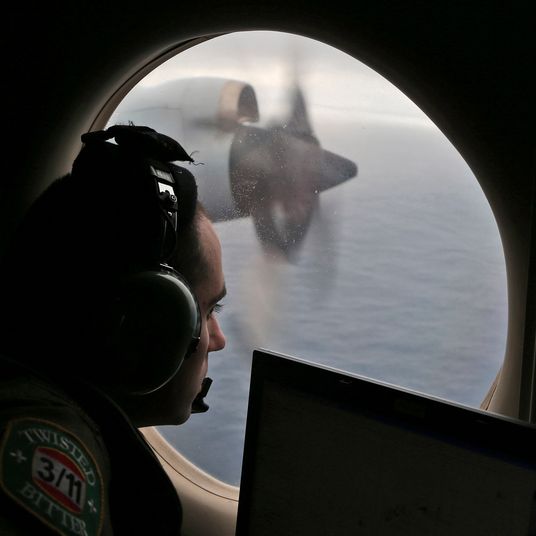
This subvariant is a recombinant of two strains, BA.2.10.1 and BA.2.75, that has been particularly prevalent in Southeast Asia, where its growth advantage over BA.5 has been substantial. So far, XBB only accounts for a handful of U.S. cases. Early data shows that it has a similar growth advantage to BQ.1, but for the most part, it and the BQ lineage have been rising in different parts of the world independently.
One lab study found that XBB had the most immune evasion of any variant yet seen, prompting some scary hyperbole in news headlines. But the early data from Singapore, where XBB now accounts for more than half of the country’s new infections and is driving a wave of cases, does not indicate that it causes more severe illness than other strains — at least not among that population, which is well vaccinated and well boosted.