Preventing entry
Understanding the body's defence mechanisms
Defence mechanisms help the body protect itself against the entry of microorganismMicroscopic (too small to see) organisms, such as bacteria and viruses that cause communicableA disease that can be passed from one organism to another..
These include:
the skin, which is a barrier to microorganisms
mucous membranes in the nose, ears, and eyes which trap microorganisms
blood clotting, which stops blood escaping and prevents the entry of microorganisms where the skin has been damaged
If a microorganism does enter, white blood cells will kill them.
The entry of a microorganism may cause us to be sick while our body fights the infection.
Antigens and antibodies
All cells have markers on their surface called antigens that have specific shape.
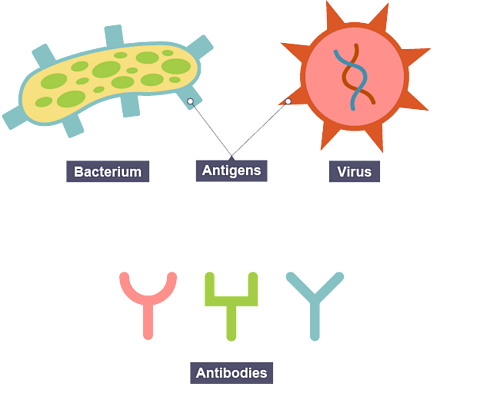
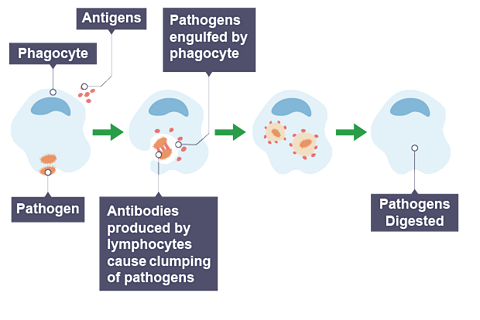
When the body recognises a foreign antigenA marker on a microorganism that causes the body to produce antibodies. on apathogenMicroorganisms that are harmful to humans., lymphocytes (white blood cells) produce antibodyA chemical produced by a lymphocyte in response to an antigen., which are complementary in shape to the antigen.
An antibody will only work on one type of microorganism because of this complementary shape.
Antibodies immobilise microorganisms by clumping them together.
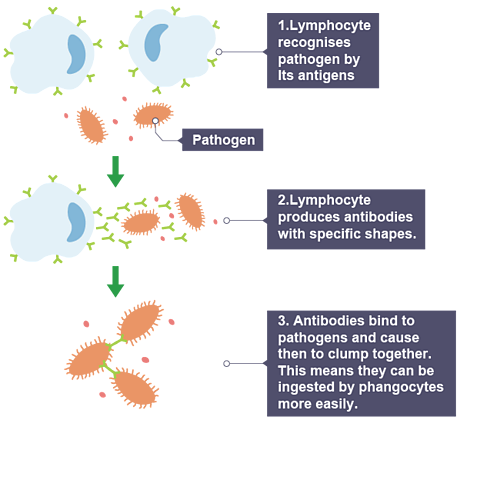
Immobilisation of the microorganism reduces symptoms and prevents the spread of infection.
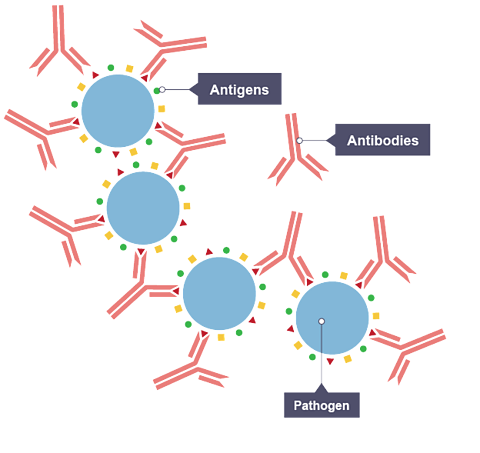
The clump of microorganisms is then destroyed by phagocytosisThe process of the ingestion of bacteria or other material by phagocytes..
Phagocytosis is when a phagocyte (white blood cell) engulfs and digests the microorganisms.
Enzymes within the phagocyte digest the microorganism.
Primary and secondary responses
The infected individual will be sick while lymphocytesWhite blood cells which attack pathogens by producing antibodies. work to produce enough antibodyA chemical produced by a lymphocyte in response to an antigen. to provide immunity.
This is the primary response.
During this response, the body will also make memory lymphocytes that remain in the body for years.
If the same pathogen is encountered again, memory lymphocytes produce high numbers of antibodies very quickly.
This is the secondary response and it prevents the person getting sick again from that pathogen or disease.
The person is now immune from that disease.
Immunity
Immunity means your body can fight off a disease. This happens when you have enough antibodiesProteins made by white blood cells that are specific to an infection. They help fight off the illness., which can protect you from getting sick from that disease.
There are two types of immunity:
Active immunity
This is when the body’s lymphocytes are activated and produce the specific antibodies needed to fight the pathogen.
Active immunity is:
slow acting
provides long-lasting protection
The primary response when a microorganism enters the body is described as natural active immunity.
vaccineA substance that stimulates the body to produce antibodies to provide immunity against a disease. provide artificial active immunity.
Passive immunity
This is when ready-made antibodies, from another source, are introduced to the body.
Passive immunity is:
fast acting
only lasts a short period of time (no memory lymphocytes are made)
Breastfeeding provides a baby with natural passive immunity.
Anti-venom provides artificial passive immunity after a poisonous bite.
Active immunity - vaccinations
How do vaccines work?
A vaccination is the injection of dead or weakened pathogens.
They stimulate the immune system to produce antibodyA chemical produced by a lymphocyte in response to an antigen. and memory lymphocytesWhite blood cells which attack pathogens by producing antibodies..
If this pathogen is encountered after the vaccineA substance that stimulates the body to produce antibodies to provide immunity against a disease., the memory lymphocytes will produce large numbers of the antibody very quickly, so the individual does not get sick.

What are booster vaccinations?
Sometimes a booster vaccination is needed to maintain the high levels of antibodyA chemical produced by a lymphocyte in response to an antigen. needed to provide immunity.
Given to maintain or increase antibody levels over time.
Ensure long-term immunity by reactivating memory lymphocytesWhite blood cells which attack pathogens by producing antibodies..
Interpreting antibody graphs:
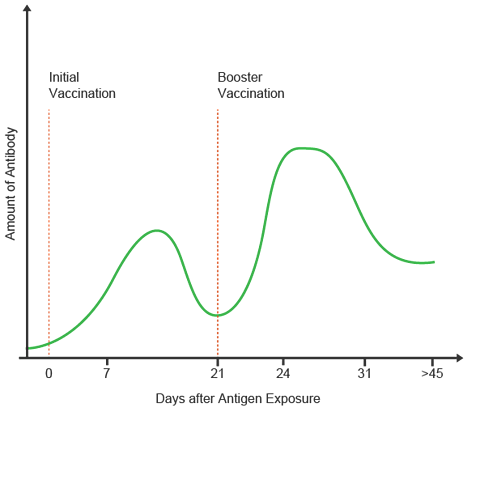
Show a rapid antibody response after boosters due to memory lymphocytes.
Highlight how antibody levels decline over time without boosters.
The development of medicines
Watch: How medicines are developed
Penicillin
Antibiotics are chemicals produced by fungi that kill or prevent the growth of bacteria.
Penicillin was the first antibiotic. It was discovered by Alexander Fleming in the 1920s when he noticed that bacteria didn't grow near a mould contaminating his cultureIn microbiology, a colony of microbes, typically on an agar plate..
He concluded that the mould released a substance that prevented bacterial growth.

In the 1940s, scientists Florey and Chain produced pure penicillin and began large-scale production of penicillin.
Since then, many more antibiotics have been discovered.
Penicillin and other antibiotics are produced commercially where fungi are grown in carefully controlled conditions (correct temperature, pH and nutrients) in fermenterA tank containing nutrients, which is used to grow large numbers of bacteria or yeast..
What are medical trials?
Preclinical trials
Before a new drug can be made available for public use, it must undergo rigorous testing to ensure it is safe and effective.
There are various stages:
1. Preclinical Trials:
- conducted in laboratories
- drug is tested on cells, tissues, and animals
- checks if the drug is toxic (poisonous) and how effective it is
2. Clinical Trials:
- drug is tested on small number of healthy volunteers first, then a larger group
- aim to find the optimum dosage that balances effectiveness and safety (no harmful side effects)
- then the drug is tested on small number of sick people to ensure it works
3. Peer Review:
- research is reviewed by other scientists before publication
- ensures the findings are valid, reliable and meet scientific and safety standards
If these trials are successful, the drug can be licensed for use.
Antibiotics
Antibiotics are chemicals/drugs used to treat bacterial infections.
Practical 2.3
Investigate the effect of different antibiotic discs on the growth of bacteria
Procedure:
- Using the aseptic technique, add bacteria to a Petri dish.
- Soak small filter paper discs in each antibiotic A, B and C.
- Place the discs apart on the bacteria in the Petri dish.
- Incubate at 25°C (safety - to ensure no pathogens grow) for 1-3 days.
- Measure the radius/diameter of any clear zones around the discs.
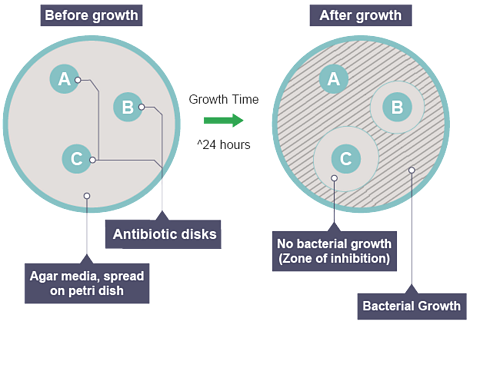
Results
C is the more effective antibiotic at killing or preventing bacterial growth because it has a larger clear zone.
Antibiotic-resistant bacteria
Some bacteria have developed resistance to antibiotics, meaning the drugs can no longer kill them.
The overuse of antibiotics is responsible for this process by allowing bacteria to mutate and become resistant.
Certain bacteria, known as superbugs (eg MRSA), are resistant to multiple antibiotics, making infections caused by them difficult to treat and posing serious health risks.
Reducing superbugs
Hygiene: regular handwashing and cleaning hospital environments.
Controlled antibiotic use: prescribe antibiotics only when necessary.
Isolation: keep patients infected with ‘superbugs’ separate to prevent spread.
Why superbugs are hard to eradicate:
bacteria can mutate quickly
resistant strains survive and multiply
limited development of new antibiotics
Plant defence mechanisms
Plants have also developed defences against infectious microorganisms.
Structural defences
Waxy cuticle to prevent pathogens entering the leaf.
Thick cell walls to prevent pathogen entering the cells.
Chemical defences
Plants can produce chemicals that kill infectious microorganisms (bacteria/viruses/fungi).
Antimicrobial chemicals kill or inhibit bacterial growth (eg antimicrobial chemicals produced by mint can kill or reduce the growth of bacteria).
Poisonous chemicals deter herbivores such a slugs (eg digitalis, a chemical made by foxgloves is poisonous to slugs and other animals that feed on it).
Quiz time!
Watch: How have humans adapted to protect themselves?
More on Health, diseases and micro-organisms
Find out more by working through a topic
- count4 of 4

- count1 of 4

- count2 of 4