
After two days of heavy rain, the evening of March 11 has turned dry and, for the season, lovely: warmish, with a waxing quarter moon. Arriving for her shift at 8 p.m., Christine Cassidy, the senior attending physician in the emergency department at Jacobi Medical Center, suspects this will mean a busy twelve hours: The nicer the weather, the greater the trauma. And this being a Friday—a harbinger of mayhem in the North Bronx neighborhoods Jacobi serves—she is not surprised, as the night wears on, to find the three trauma bays steadily stocked with stabbings and gunshot wounds, while the rest of the emergency room deals with the heart attacks and strokes and mystery fevers that fall within its domain. Even on ordinary weekends, the Jacobi trauma center, often the busiest of the seventeen Level 1 centers in New York City, is something of a war zone: ambulances, police, bodies, blood. And this is no ordinary weekend.
At about 3:45 a.m., a World Wide Tours charter bus leaves the Mohegan Sun casino in Connecticut, a bit more than two hours from the Bronx. Many of the 32 passengers are Chinese-Americans heading back to Chinatown, where the trip originated on Friday evening. They have spent the interim gambling, eating, and generally enjoying themselves. The round-trip, including vouchers for food and slot machines, cost $15. A Chinatown sign advertising the tours says, “Go with the wind, be prosperous.”
Whether Ophadell Williams, the driver, is speeding or has perhaps fallen asleep at the wheel will surely be argued in the lawsuits being brought against him and World Wide Tours. Williams maintains that while crossing into the Bronx on I-95, he is clipped by an improperly passing tractor-trailer. In any case, witnesses, including some surviving passengers, say the bus swerves repeatedly onto the shoulder, rattling the rumble strips at the edge of the pavement, in the moments before it flips onto its side near exit 14 for the Hutchinson River Parkway. Once on its side, it hurtles forward another 480 feet and plows into a stanchion supporting the exit sign. The stanchion slices through the top of the bus from the front almost all the way to the back, at mid-window height—head level—peeling the roof back like the lid of an anchovy tin and carving through whatever it encounters on the way.
It is now 5:35 a.m. When EMS workers arrive moments later, they find a sickening scene, with a severed head and severed limbs, people hanging upside down, screaming, darkness, glass, and blood. Amazingly, they manage to pry bodies from the twisted metal and from each other; sort the thirteen dead from the twenty living, if barely so; and dispatch the first ambulances before 6 a.m.
The squat red phone with no dial or buttons rings at the nursing station. All Cassidy is told is that two patients, victims of a bus accident, are on their way. Based on this scrap of information, she puts out a Level 2 trauma call. But when the ambulances roar up minutes later—the accident was a mile away—she takes one look at the patients and begins to reconsider. “How many more?” she asks the EMS worker.
“A lot. The bus was destroyed.”
Awaiting the trauma team, she and the junior attending physician try to stabilize the first two patients. Cassidy also starts planning for a much larger disaster. Regular emergency patients will have to be cleared out, trauma equipment rushed in. She ups the call to Level 1 as victims keep arriving. Before an hour is up, there are fifteen.
Sheldon Teperman, head of Jacobi’s trauma service, is compulsive, “like Batman,” about being reachable. When his cell phone rings at 6:30 a.m., he’s in bed at home in Hoboken, New Jersey. Briefed on the situation, he throws on his jeans and “levitates” to the hospital, making a trip that can take an hour in 23 minutes. He tells himself: Do not get into an accident. He slows down on curves.
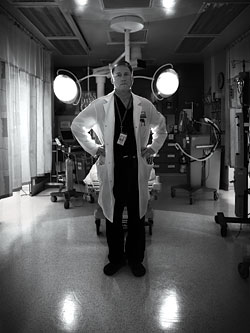
Teperman is 50 but looks younger, with blondish hair and blue eyes. In his peacock-blue scrubs he projects the swagger of a person who was accepted to medical school at age 17. This confidence is desirable in a traumatologist. Though the team has trained relentlessly, including mock incidents with euthanized pigs standing in for humans, the residents have never dealt with a disaster on this scale and have delayed most major decisions until Teperman can weigh in. When he arrives, Cassidy says to herself, Thank God.
By now the fifteen patients are situated in bays with a team assigned to each. Seven have injuries that can wait a bit. But eight are wildly unstable; there are blunt chest traumas, multiple fractures, head injuries, ruptured organs, massive internal bleeding, missing limbs, and a patient whose severe criticality cannot immediately be explained. Several desperately need surgery, but the only operating room typically available on the late shift still has a gunshot victim in it.
Rounding the floor, Teperman is reminded of the Little Chester shoe-store massacre in 1995, when a man opened fire, killing five and injuring three. Jacobi treated the victims, but this disaster is an order of magnitude worse: a “shit storm,” he says, “a textbook of trauma in one day.” And not just because of the number of casualties, though fifteen at once is huge even at a Level 1 center. Jacobi admits 1,900 trauma cases a year. About 21 percent—a very large portion—are “penetrating” traumas, mostly gunshots and stabbings. The rest are “blunt”: car accidents and falls as well as more deliberate blows. The bus victims have both kinds, and Teperman is further troubled by the strange addition of wounds caused by shearing. They never tried that combination with pigs.
Teperman uses the word sick the way laymen would say “dying.” One woman is severely hypotensive, with bleeding from midface injuries and trauma to the chest. But she isn’t—yet—as “sick” as some, and the source of her problem is not clear.
So he turns his attention to a man whose blood pressure is dropping precipitously. He has rib fractures, many blunt injuries, and some sort of brain trauma. He is running out of time. A sonography exam finds bleeding in his abdomen—but where exactly? The scan doesn’t name the organ.
Teperman sends the patient to an operating room; several are now up and running. There, Peter Kim, an attending surgeon, opens him up. The bleeding is coming from the spleen. That’s luck; you can live without a spleen. Kim contacts Teperman. Given the need to keep operating rooms available for more critical patients, should he wait? No, Teperman says: “Whack it.” Kim throws down the clamps, cuts out the organ, sews the surrounding vessels.
“Once the clamps are on, the game is won,” Teperman says. “He’s dying, dying, dying, and then he’s saved.”
Saved for the moment; his broken ribs and brain injuries remain to be dealt with. But others need more immediate attention.
“People are constantly trying to die on me,” Teperman says. “It’s very annoying.”
A victim whose arms were sheared off by the stanchion, the tissue and bone “pulled, torn, and gouged up,” is sent to the OR. The wounds are cleansed and the amputations “revised”—cut back to healthy tissue so they can be prepared for closure and the acceptance of prostheses later.
Meanwhile, another man, with multiple fractures, is in very bad shape. A CAT scan shows that he is bleeding from the pelvis. Doctors fit him with a T-Pod, a corsetlike binder commonly used in battlefield incidents involving improvised explosive devices. By stabilizing the area, the T-Pod can often stop the bleeding, but this time it doesn’t. Once again the question is, where exactly is the blood coming from?
In the interventional radiology suite, radiologist Conway Yee tries digital X-ray fluoroscopy to pinpoint the source. He inserts a micro-catheter through the femoral artery, threads it carefully into the pelvis, then injects a dye and studies the screen. If blood is leaking from vessels, the dye will make it visible. He looks everywhere, but there’s nothing. He asks Teperman what he should do; Teperman says to try again, fast. “And even if you don’t see anything this time, take out the big feeding vessels.” Neither the patient nor Jacobi can afford any more bleeding.
Yee performs a second run, injects the dye—and there it is. A ruptured vessel, leaking black on the screen. Tiny surgical tools inside the catheter allow him to disable it without damaging larger vessels. Next he inserts a “gel foam” that instantaneously seals the cut ends. Another injection of dye shows no further bleeding. The man is saved; his vital signs become “rock stable.”
Despite the TV-ready clichés—shock paddles, blood spouts, adrenaline injected into hearts—the emergency floor is strangely calm. Four hours in, more than 100 staff are working feverishly if quietly on the fifteen patients. (Another five, including the driver, were taken to St. Barnabas Hospital, several miles farther west.) Trauma centers don’t get much glory; no one peruses a best-doctor list to decide where to get shot or run over. But Teperman feels confident enough of his team’s response to think, for a moment, that the situation is under control.
It’s true that the patients are unusually quiet. Removing the dressing on an open fracture, a procedure that would ordinarily produce a scream, produces nothing. Some of course are not even conscious, but even those who are seem astonishingly stoic. Or are they simply too shocked to understand what’s going on? Having been told that the most severely injured patients are Cantonese, Teperman takes a Cantonese-speaking resident to each bedside and has him say, “You’re in a hospital, you’ve been in an accident, you’re going to be fine.” Mostly, they do not respond.
And who are they? Many arrived with their clothing torn off; EMS workers did not go searching for wallets. Because of their traumas, some will not even be recognizable to their families at first. One will turn out to be homeless, reportedly using the bus as a way to stay out of shelters.
In some ways, their identity doesn’t matter. In his career, Teperman has worked as hard on old ladies caught in gang crossfire as on the gangbangers themselves. The job is the same, whoever is on the table. In another way, it matters very much. Trauma is something that happens not just to the victims but to their families, and even to their doctors. Soon the circle of the accident will widen. Identifications will have to be made, survivors counseled. All of that will be complicated by cultural sensitivities. Some Chinese do not want to associate themselves with what may look to outsiders like an endemic gambling problem.
But before social workers can address all this, a second wave of instability swells.
A female patient with abdominal trauma enters the “triad of death”: hypothermia, acidosis, coagulopathy. (Her body temperature is low; her blood is acidic and won’t clot.) Dr. Kim, fresh from the splenectomy, opens the woman. She’s bleeding from the liver and elsewhere in the abdomen. He manages to control that flow, but there is a lot of nonsurgical bleeding, and her vital signs do not respond. She is still in the triad.
When Teperman was training, surgeons would have kept operating on a patient like this until she died. Or she might have died already, because trauma centers had not yet learned to transfuse separate blood components, which include clotting factors, as early as possible, nor to warm the blood as it came out of the fridge. With improved protocols in place, Teperman feels the patient has a better chance if they “temporize”; Kim packs the abdominal cavity with towels to stanch the bleeding, covers the opening with plastic wrap, makes a temporary closure with a suction device, and leaves the rest to nature “so she can live to fight another day.”
And that’s exactly what happens. With the damage-control procedure completed, the patient starts to reconstitute quickly. When the wrapping and towels are removed 24 hours later, she is fine.
But the woman who arrived hypotensive, and whose exact problems have still not been determined, lies dying on the table. She needs constant transfusion. The “Shel Saver”—the trauma service’s prized reserve of blood, named for Teperman—is empty. In all, hundreds of units are used. Teperman runs down the hall to the bank for more.
He has been cycling like this from the bank to the trauma bays to the operating rooms since he arrived hours ago. Now, as he returns with more units, he regrets not going to the gym as much as he used to. Winded, he simply throws the blood at his colleagues and drops to the floor.
On his knees outside the OR, he talks through the case with Melvin Stone, a critical-care surgeon, who then starts an emergency thoracotomy and blunt dissection of the aorta. But the procedure is tricky—in a nonemergency situation, it can take an hour—and the woman is about to die. Because Teperman often performed it on gunshot victims during the crack wars of the eighties, he scrubs in and takes over, finishing the job in less than two minutes.
Still, twenty minutes later, she’s coding again. Stone says, “Should we stop?”
Later, Teperman keeps replaying that moment. “An old professor of mine used to say when you’re a surgeon and a Jew, you’re guilty squared.”
They don’t stop, but she dies anyway.
When is a trauma over? By 1 p.m. Saturday the victims are cleared from the trauma bays and are being cared for elsewhere in the hospital. But for the doctors, is it when they get to leave? As soon as Cassidy, after fifteen hours on duty, feels that the surviving survivors are “tucked in,” she heads for home. But her car breaks down on the Hutch.
Teperman doesn’t get back to Hoboken until late Sunday morning, and then, just as his head hits the pillow, his phone rings again. Mayor Bloomberg is to hold a press conference at Jacobi in which he’ll plead for help in making a final identification. Teperman drives back, this time not speeding.
It might be considered a miracle, or at least a victory, that of the fifteen patients brought to Jacobi after the worst bus disaster in the city’s history, fourteen survived. (Four of the five brought to St. Barnabas, including the driver, survived as well.) But two patients remain at Jacobi months later; the homeless man is still homeless. And Teperman still grieves for the patient he lost.
“A surgeon should never take a bow except when his patients die of old age,” he says.
Even for those who were saved and sent home, Teperman is painfully aware that the trauma is far from over. There will be years of pain and procedures, disability and nightmares. In effect, what he and the rest of his team have done is save them so they can be saved by others, again and again, for the rest of their admittedly longer lives.