It was the last week of the longest March in recorded history, and Mount Sinai Brooklyn was teetering on the brink of collapse. In the emergency department of the 212-bed community hospital in Midwood, more than 90 patients were crammed into a space that usually holds 30 or 40. Almost every one of them was short of breath. Emergency-room nursing director Bobby Lynch played a complex game of Tetris to extricate a patient from behind a five-deep row of stretchers, maneuvering him to one of the three dialysis-equipped bays, while department medical director Deborah Dean rushed to bring a portable oxygen tank to a patient whose skin was turning blue. The alarms indicating patients who required immediate resuscitation rang out in a deafening trill. Corpses lay under white sheets head to toe with the critically ill. Roughly a fifth of the hospital’s staff was sick with COVID-19, including the hospital’s president, Scott Lorin, who was coordinating reinforcements from a stretcher in Mount Sinai’s main branch on the Upper East Side. And according to the governor’s office, it was going to get worse. “We just looked at each other, and one of my co-directors said, ‘If this isn’t the peak, I’m afraid of what the peak will look like,’ ” Lynch recalls.
Lorin, 51, had been a pulmonary and critical-care physician for 20 years before becoming an administrator. He knew intimately how overextended his hospital had become. Pre-COVID, the ICU could hold 12 patients. On April 1, 51 patients were on mechanical ventilators, and around a third of the patients in the hospital required critical-care support. That same day, 37 rapid-response teams were called; on a normal day, it’s around three. As he described the situation to his bosses, he periodically hit mute to cough and gasp for air. “My job is to see the future,” he says. “And I saw [our numbers] rising so fast, and us so unable to keep up, that the hospital was really in danger.” His worst fear was that people would begin to die, not just because of the virus breaking down their bodies but because of a hospital that had broken down around them. “There is no blueprint for that at all,” Lorin says.
In the end, the hospital didn’t collapse, and now, as the first wave of the pandemic recedes, Lorin and his staff are conducting what’s known as a “hotwash,” a systematic evaluation of how they weathered the crisis. The virus was a stress test for the medical system, finding its weaknesses but also summoning its strengths. COVID wasn’t a single tsunami that pummeled MSB; rather, it was “crests after crests, day after day, waves and waves of tsunamis,” says Lorin. “It’s not that you’re making rapid, courageous decisions or actions for a few days; you’re doing it every day, and it’s constantly evolving.” They learned a lot.
The virus hit Mount Sinai Brooklyn early and hard. That it survived without seriously rationing care or a complete breakdown is no small feat. It did so in part due to quick decisions on the individual level and a bureaucratic hospital system’s embrace of flexibility. The job for Lorin now is to understand what made the difference, so that when the virus comes again, which in all likelihood it will, they’ll be ready.

Mount Sinai Brooklyn opened its doors in 1955 as Kings Highway Hospital, serving the primarily Jewish community in South Central Brooklyn. Community hospitals traditionally handled lower-acuity conditions that still required inpatient stays. People came for a burst appendix or a broken limb, chemotherapy or dialysis treatments.
In the past few decades, hospitals like this have seen their patients siphoned off by both urgent-care clinics and large academic medical centers, the kind equipped with state-of-the-art technology that can take care of sicker patients and, just as significant, command higher insurance reimbursements. Many smaller hospitals have either folded or been absorbed into larger health-care systems, including Kings Highway; in 1995, it was bought by Beth Israel Medical group, which became part of the Mount Sinai Health system in 2013. Mount Sinai is now the largest academic medical system in New York City and one of the biggest in the country, with eight hospitals, a medical school, and around 150,000 inpatient admissions per year.
Still, Mount Sinai Brooklyn remains at its core a community hospital. Staff often live in the surrounding neighborhoods, and some have treated the same families, who now include Russian immigrants as well as African- and Caribbean-Americans, for decades. While the hospital has new facilities, like a robotic-surgery center, the sickest patients are generally transferred to the main Mount Sinai campus. MSB’s East Wing, with its narrow corridors and cramped patient rooms, dates from the 1950s and has none of the glamour of the Manhattan hospital. “The type of doctors who retain PR agents aren’t the type to come and work in Midwood, Brooklyn,” says Gary Gwertzman, MSB’s director of vascular surgery, who has been there for 14 years. “When there is a major medical event in the world, CNN doesn’t come to Mount Sinai Brooklyn, and the folks here are fine with that.”
The affiliation gave MSB significant advantages in fighting COVID. For one, a sourcing team began working in January to build up stores of PPE, even sending two private jets enlisted by Warren Buffett’s company to get N95 masks from China. That meant that at the peak of the crisis, even while public hospitals faced PPE shortages, Mount Sinai’s remained stocked. But for all that, the virus kept surprising them, to deadly effect, behaving like nothing they had ever prepared for.
“The major issue, looking backward, is that in the beginning we were admitting COVID -positive patients in the hospital and we had no idea,” says Lorin. The initial directive to all Mount Sinai hospitals was to screen for patients with respiratory issues who had a relevant travel history.
In mid- and late February, the hospital ran “secret shopper drills” in which Lynch and Dean hired their family members to come in complaining of cough and fever and admit they had traveled to affected areas only if the staff pressed them. If staff uncovered this information, they had been trained to isolate the patient in a small area of the ED that had been sectioned off.
At this point, the hospital was testing only patients with respiratory complaints, and it was a convoluted process: For people tested in the ED, test kits were sent out to LabCorp, and five days later results would come back. Patients admitted to the hospital were tested through the New York State Department of Health, which had to approve the test and then had a two-to-three-day turnaround. On March 9, a patient was admitted complaining of dizziness. ER doctors ordered a CT scan and were shocked to discover his lungs were filled with COVID’s telltale ground-glass opacities. It was the hospital’s first confirmed case.
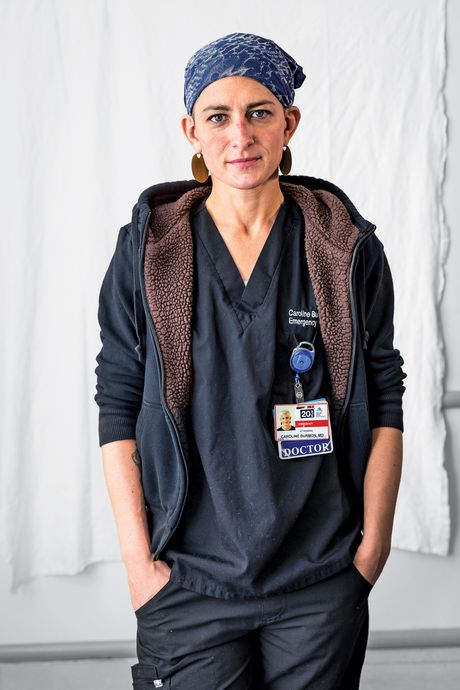
Over the next week, as the ED staff increased testing, they discovered that patients who came back COVID-positive were complaining of everything from diarrhea to neurological issues. And only a few of them had been to Italy or China. On March 16, Lorin had a conference call with all his ER physicians and told them to throw away the existing criteria for testing. This was around the same time the hospital got the green light to do testing in-house, which meant they could test everyone in the ER, as well as their own staff, and results would come back within 12 hours. The number of positive results began doubling almost daily. “We were exposed to this medical knowledge live,” says ED doctor Caroline Burmon. “Physically as well, our exposure was absolutely outrageous. And there were no warning bells from the government for us to follow. It was all on us.”
The hospital was quickly becoming all COVID, all the time. The ED was so overloaded that on March 19, a 12-person tent was added outside to treat low-acuity COVID cases. By the second half of March, Lynch had called the city five times to ask that EMS stop bringing in new patients. But EMS had no choice; every other hospital in the area was full too.
On the last weekend of March, the hospital’s chief nursing officer tested positive. With Lorin still out sick, chief medical officer Peter Shearer was the only member left of the clinical leadership team. “I knew we needed to call in the cavalry,” says Lorin.
The cavalry turned out to be led by Linda Valentino and Michael McCarry, two senior nurses from the main campus. Valentino had worked as MSB’s chief nursing officer before heading nursing operations at the main branch. She would be “incident commander.” McCarry, a Belfast-trained nurse who had helped lead Mount Sinai’s relief efforts after the Haiti earthquake, would be acting COO.
One of their first tasks was to refashion the hospital’s spaces to protect the staff from getting sick. The initial plan to have a separate area for COVID patients had long been abandoned, and the entire hospital was essentially a “red zone,” a space with a high risk of contamination. “I said, ‘The whole staff can’t be a red zone.’ Staff have to function. Because people were hysterical,” says Valentino.
She and McCarry, along with an infection-control team, divided the hospital into green, yellow, and red zones, depending on the risk of contagion; these were marked by signs and tape. They relocated the PPE to an enclosure at the front door of the hospital to ensure that the staff had fresh scrubs every day and that everyone received N95 masks whether they were directly dealing with patients or not. Their goal was “to pump resources or structure into the place as quickly as possible,” as McCarry puts it. “But the main resource that was needed was people.”
Many of those came through volunteers from the rest of the Mount Sinai system. With nonessential surgeries canceled systemwide, there were many underutilized people with the technical skills to manage critical-care patients, even if they hadn’t drawn on those skills in years. Michael Marin, the Mount Sinai system’s surgeon-in-chief, made a list of every free hand and organized them into groups he called platoons. Each was led by a senior surgical resident. Even though the surgical residents weren’t the most senior physicians on the team, they had more recent hands-on experience in an acute-and-critical-care setting.
One platoon recruit was Dan Herron, chief of bariatric surgery at Mount Sinai Hospital uptown, who was used to commanding a team and teaching fellows. Now he found himself rolling gurneys down the hall, changing soiled bedsheets, and disconnecting oxygen tanks. “Traditionally, in a hospital that’s operating within its normal capacities, everyone has clearly defined roles, but there were kind of no boundaries in my time there,” he says. “Everybody just did what needed to be done.”
In addition to the 150 or so volunteers from within the Mount Sinai system, more than 90 temporary workers began flooding in from around the country. “There were times you would introduce yourself and ask someone where the lab is, and often the response you’d get is ‘Oh, I just showed up today from Minnesota,’ ” recalls Herron. It took Shearer a few days to know what to do with the random assortment of nurses, cardiologists, and gastroenterologists, but he learned to see the new staff as pieces of a puzzle; slotting them into the right place sometimes required turning them in a different direction. Some of the more experienced doctors were instrumental in helping him organize the many patients they began transferring out to other hospitals. Gwertzman, who had spent more than 20 years doing complex surgeries on arteries and veins, was teaching PAs how to insert lines on critically ill patients, and floor nurses were pivoting to do the work of critical-care nurses, learning how to titrate the array of medications required by intubated patients.
To bring them in quickly, the hospital had relaxed its vetting procedures. The results were mixed. A few complained to McCarry about being sent to Brooklyn when they thought their assignment would be at the fancy teaching hospital uptown. Some were overwhelmed by all the stress and death and quit early. “The rule of thumb was that one out of three is not going to survive here,” said Lorin.
Meanwhile, the members of the hospital’s medical team were rewriting guidelines on a daily basis. As new drugs came into vogue, they were integrated into treatment, only to be phased out when studies showed their promise was illusory. Early on, doctors were sometimes intubating patients when their blood-oxygen readings seemed to indicate they were about to crash, even if they were still wide awake and talking. But one of the unusual effects of COVID was that patients seemed able to tolerate alarmingly low blood-oxygen levels—numbers that would normally prompt intubation—while the stiffness of their lungs made pushing air in via the mechanical ventilators much more difficult, like trying to inflate a steel balloon. For these patients, “taking away their respiration and awareness and homeostasis was actually more harmful than anything,” says Burmon.
By early April, it was clear the sickest patients on ventilators were unlikely to come off them. The staff began opting for less invasive ways of providing oxygen when they could, like bipap masks and high-flow nasal cannulas, which they had resisted initially partly over concerns that these methods would aerosolize virus particles. But better infection-management procedures helped them rethink their protocols.
“The hardest part was realizing there wasn’t much I could do. It took all these years of learning and pattern recognition and all the knowledge and skills I have, and it made them useless,” says Burmon. “I think a lot of people were struggling with that, but I’m not sure there was ever any acceptance of it, and that might be a good thing. People are still trying to innovate and think of the right way to treat people.”
The arrival of new staff provided enough muscle to “prone” patients in the ICU, i.e., flip intubated patients onto their stomachs to allow more oxygen to enter the lungs. McCarry got a bunch of proning pillows from the main Mount Sinai, and a team of techs that had been brought in to hand out PPE doubled as the hospital’s proning team. It took four to six of them working together to turn one patient onto his or her stomach while making sure all the tubes and intravenous and arterial lines stayed secure.
And the death toll kept rising. On March 31, there were eight confirmed COVID deaths. On April 1, there were 17, and on April 3, 20. By then, the hospital had turned perioperative rooms into a second 11-bed ICU. Even then, there were often 20 to 30 patients receiving intensive care in other parts of the hospital.
Valentino and McCarry spent a lot of time figuring out how to organize the two morgue trucks parked outside the hospital. At one point, 65 bodies were waiting to be claimed. For Valentino, caring for the bodies in a respectful way felt essential. They created a system to account for personal effects, so that when someone called looking for his grandfather’s wedding band, they knew where to find it. “We have the dubious honor among the funeral parlors of having the best organized trucks in Brooklyn,” McCarry says.
Staff who had never made calls to patients’ families suddenly found that much of their job involved telling people their loved ones had died. Shani Goldman, an orthopedic PA who was rerouted to the ICU, went from resetting broken bones to managing drips and ventilators. “Normally, I call people and I tell them, ‘Your mother broke her hip; we’re gonna fix it tomorrow,’ ” she says. “Now I was calling the patients’ families to tell them that, in 24 hours, we think your father or daughter or sister or brother is gonna die.” For many of the critical-care staff, the hardest part was watching patients die alone without their families beside them. “We put many, many, many patients in body bags. I had never touched a dead person before,” recalls Goldman.
Palliative-care specialists arrived to ease the burden. Valentino also introduced her nursing staff to “the pause,” a 45-second moment of reflection after a death, as a way to honor both the patient and the staff. Nurse manager Melinda Cotterell-Russell remembers thinking it was something she would never actually use. But that night, her unit had ten deaths. After they called time of death on the third patient, she asked the staff if they could stop for a second. “I said, ‘Let us take a moment to pause and honor Mr. Jones.’ ” A silence fell over the room, and she could hear her colleagues breathing. “It gave them the strength to go on to the next patient. And it has been working since.”


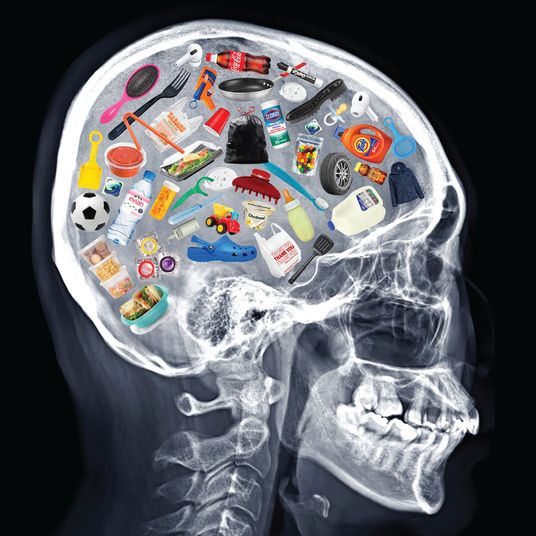
By this time, it was becoming clear that COVID was a pathology not only of the lungs. At first, Gwertzman, the vascular surgeon, had wondered what role there would be for a veins-and-arteries guy amid a viral-pneumonia outbreak. But almost immediately, he was seeing COVID patients with severe clotting. One of his COVID-positive patients had no other symptoms, but when he finally came in complaining of leg pain, he had such a bad blood clot that Gwertzman had to amputate. Meanwhile, people in their 30s and 40s were coming in with strokes, a result of blood clots in the brain.
The disease was in the blood, which explained why symptoms showed up in so many parts of the body. By the time a study came out of the main Mount Sinai describing the clotting phenomenon and recommending blood thinners as a possible course of treatment, the staff at Mount Sinai Brooklyn had already been using them on select patients.
Another big surprise for the clinical team was the number of kidney failures they were seeing. When the crisis began, the public worry was a shortage of ventilators, but they ended up having more than enough. The hospital had leased ten additional ventilators in early March, then received another 47 from the main Mount Sinai. By late March, they had 86 machines, and with elective surgeries canceled around the country, it wasn’t hard to recruit anesthesiologists and CRNAs who knew how to intubate patients. The more challenging shortage ended up being dialysis. Many critically ill patients developed acute renal failure, but it was hard to find enough of the more specialized dialysis-trained staff. At one point, a frustrated Gwertzman tweeted at Elon Musk, asking him why he was sending ventilators when he should have been sending dialysis machines. (Musk didn’t respond.) To service all their patients on the existing machines with the staff they had, some who would normally have received dialysis four times a week received it only two or three times a week.
Lorin’s first day back to work was April 6. He had been gone for only two weeks, but so much had changed. Above patches of chafed skin along the edges of their masks, his staff’s eyes radiated anxiety. They told him how their bodies were sore at the end of the day from performing so many chest compressions, how they hadn’t seen their families in weeks, how they were worried about getting sick like their colleagues. They didn’t know it yet, but for MSB, the wave of the pandemic had already crested. By the second week of April, admissions were steadily falling. Some nurses and doctors from out of state were preparing to take the lessons they had learned back home, while Marin’s platoons had been transferred to other hospitals in the system.
Many of the top brass at Mount Sinai tout the crisis management at Brooklyn as an example of the system working as it should, one big interlinked family sharing knowledge and resources. “If Mount Sinai Brooklyn was still independent, it would have collapsed,” says Lorin. “I have 100 percent certainty of that.” Seeing how they could create flexibility within a typically rigid organization was one of their biggest victories.
But MSB’s good fortune also pointed out the disparities in the health-care system as a whole. Other hospitals struggled to marshal the supplies and staff they needed, and even the leverage of a large system hasn’t been able to protect staff from the specter of layoffs and pay cuts. The American Hospital Association estimates that U.S. health systems and hospitals lost an average of $50.7 billion per month during the COVID crisis. On May 13, Mount Sinai announced it was reducing pay and hours for some employees as well as ending crisis pay. To frame the story of Mount Sinai Brooklyn as a success, some staff argue, is to ignore the many ways it failed. One staff member noted that unnecessary money had been spent on visiting doctors and nurses who weren’t up to snuff. One visiting nurse was distressed that Mount Sinai had not brought in more ICU-trained nurses.
“I would consider my strength my ability to organize chaos,” says Lorin, who says the hospital brought in as many critical-care nurses as it could. “I think we found ourselves in a position where we couldn’t organize the chaos the way we’d like to. And I think everybody else found themselves in that position also, because it was so overwhelming,” he says. “I’m a perfectionist. But you couldn’t be a perfectionist. You had to do your best with what you had.”
As the immediate crisis has abated, the hospital has emptied. A few non-COVID patients have started trickling back in, but many of the usual appendicitis cases and heart attacks and strokes never returned. Lorin thinks they probably suffered or died at home.
“As things improve, you’re kind of in this state of euphoria and relief. But then once that settles down, you go into a state of bewilderment,” he says. Despite everything they’ve learned about COVID, they still can’t reliably predict who will die from the virus. And separating patients who have tested positive remains a challenge when it still takes eight or nine hours to get a COVID-test result back.
All told, about 37 percent of the hospital’s staff, more than 300 people, were out sick with COVID. Three employees have died — two physicians and one nursing assistant. Things have been so crazy that there hasn’t been time to mourn them collectively, but Lorin knows the importance of giving his staff a moment to pause. “The fact is that, God forbid, I could have more staff that will die,” he tells me. “Right now, it’s just simmering. We don’t know what’s going to happen. That’s the fear behind all of this — that it’s not over.”
*This article appears in the June 8, 2020, issue of New York Magazine. Subscribe Now!
More From This Series
- Eric Adams’s Plan to Commit the Homeless Has Little Meaning in the ER
- Working Wave After Wave at Elmhurst Hospital
- Diary of a Hospital: ‘It Felt Like a Calling’
- Diary of a Hospital: A Nurse’s Worst Day
- Diary of a Hospital: The Last Face They See Before They Die