Ever since I read Miranda July’s All Fours this spring, I’ve had a new category of health symptoms to worry about: possible signs of perimenopause, the sometimes-long, somewhat ambiguous lead-up to menopause. I’ll soon be 38, which will mean I can’t plausibly claim “mid-” 30s anymore and can be fairly called almost 40. Which is fine, except that I’m an anxious millennial — and I’m not alone. July’s perimenopausal protagonist is 45 years old; the oldest millennials (born in 1981) are now 43. We want to know this: When is perimenopause going to happen to us, and what will it be like? Here, we express the full range of our concerns, with input from physicians and women’s-health experts.
.
Many of my friends have been wondering if they might be perimenopausal lately. I don’t think I have hot flashes, and my period is fairly regular, but my sleep isn’t always great … Am I in perimenopause?
Unfortunately for the hypochondriacs among us, no blood test or diagnostic tool can definitively determine if you’ve started perimenopause or not, says Louise Newson, a physician, member of the U.K. Menopause Taskforce, and author of The Definitive Guide to the Perimenopause and Menopause. To make matters more difficult, Newson says there’s a “real blurring of lines between PMS symptoms and perimenopause symptoms” like breast tenderness, irritability, mood swings, brain fog, and decreased libido. According to Lisa Mosconi, a neuroscientist and author of The Menopause Brain, perimenopause more commonly begins in one’s early to mid-40s, though it can start earlier. If one’s period is regular, and there are few other symptoms, it might indicate early signs rather than “full-blown” perimenopause, she adds.
.
When, exactly, does perimenopause start?
Again, I wish I could give you (and me) a clear number, but it varies a lot. Mosconi says the average age at perimenopause in the United States is 47 years, but it can begin in one’s late 30s; any earlier is very rare. If you know your mother went through menopause on the early side, that might be an indicator that you’re due for an earlier menopause (and perimenopause) as well, says Shahzadi Harper, founder of the Harper Clinic and co-author of The Perimenopause Solution.
.
How long does the “peri” part last?
“On average, perimenopause lasts about four to seven years,” says Mosconi, the neuroscientist — adding that it can be shorter or longer. Tamsen Fadal, a women’s-health advocate and author of the upcoming book How to Menopause: Take Charge of Your Health, Reclaim Your Life, and Feel Even Better Than Before, notes that Black women tend to experience perimenopause symptoms for longer than white women (sometimes for ten-plus years) and may begin experiencing those symptoms earlier, too. Because perimenopause precedes menopause, defined to have started when you’ve gone 12 full months without a period, it’s easier to pinpoint the start of one’s perimenopause retroactively — which, I know, is not that helpful right now. “I look back now, and I think, Oh my goodness, I probably experienced symptoms for about 10 or 12 years,” says Newson. “But I didn’t realize because they’re quite insidious initially, and you don’t really join the dots.”
.
So what should I look for as the first sign of perimenopause?
Annoyingly, many of the earliest perimenopause symptoms are easy to overlook or attribute to other causes, says Mosconi. “Changes in sleep, mood, and energy levels are common,” she explains. “Some women notice shifts in their menstrual cycle — maybe their period is a little lighter or heavier, or the cycle length changes.”
.
Oh no. What else is going to happen?
Per Mosconi: “Not to alarm you” — too late — “but it’s not uncommon to experience symptoms like mood swings, occasional brain fog, and changes in libido. Hot flashes and night sweats may make an appearance, and some women report new issues with skin dryness, joint pain, or digestive changes.” (“Digestive changes” is a euphemism if ever I’ve heard one!)
.
I’m noticing that a lot of the symptoms you’ve described sound like what I started experiencing the second I turned 30.
Well, yes: Some perimenopausal symptoms echo general aging symptoms, says Mosconi; the difference is that hormonal changes in perimenopause makes those symptoms more persistent. Some of the life stressors common in one’s 30s (career changes, motherhood, etc.) can also cause hormonal fluctuations, adds Harper, but at some point, our estrogen levels begin to diminish and don’t come back up again. (Unless you start hormone therapy — more on that in a minute!)
That said, Mosconi offers a few words of reassurance. “Not all symptoms are inevitable or severe, and about 10 percent of women don’t report any symptoms other than menstrual irregularities,” she adds. Harper, too, notes that stress and lifestyle factors affect the severity of our perimenopause symptoms. So just … don’t stress. Ha.
.
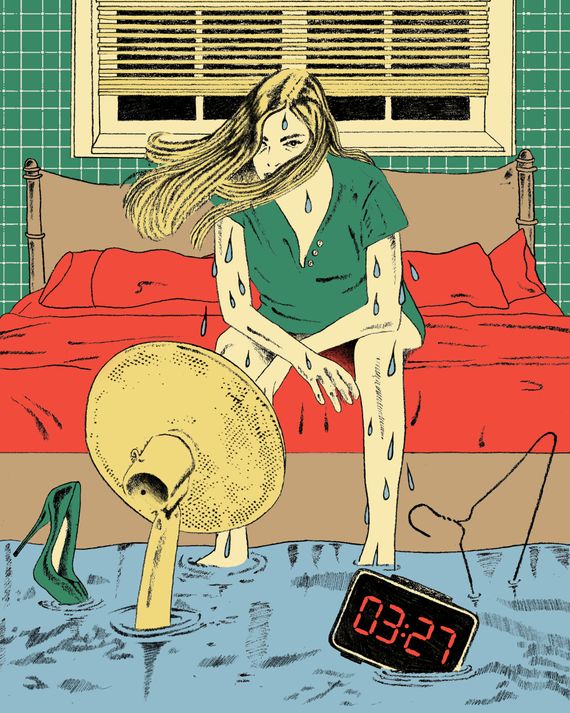
I love sleeping more than most things, and I’m afraid to ask: Will my sleep quality just get worse and worse from here on out until I die?
No! Definitely not. Perimenopause can disrupt our sleep, says Mosconi, but there are ways to combat this symptom, like “good sleep hygiene” (i.e., consistent bedtimes, earplugs and/or sound machines, wind-down time without screens, etc.) and stress-management techniques. And Newson notes that treating your hormone levels can greatly improve one’s quality of sleep: “Our hormones interact with melatonin, which is a sleep hormone. So if we have low estradiol and low testosterone and progesterone, then we have low melatonin as well. One of the first things people thank me for when they start hormone therapy is sleep improvement.” Starting good habits early also makes it easier to stick to them down the road, Fadal adds. “I was a news anchor for a long time, so I would exist on very little sleep, and I was very proud of it,” she says. “I regret that. I wish I paid more attention to that part of my life sooner.” Now in her 50s, Fadal maintains a consistent sleep schedule and says she’s getting some of the best sleep of her life.
.
Drew Barrymore tells me that my hair is going to fall out. Is she right?
Maybe. Our hormone levels do affect our hair, which is also why some (though not all) people experience thicker hair during pregnancy or other hair changes. Hair thinning and loss can happen during perimenopause, but it’s not guaranteed; not every person who goes through perimenopause will experience every symptom, Fadal explains. If you do experience hair thinning and/or hair loss, Harper notes that “maintaining a healthy diet rich in protein, vitamin D, and iron — and eating more nuts and seeds — can help.”
.
How exactly is my period going to change before it goes away completely?
How it changes varies, but changes in general are common. Mosconi says periods tend to become more erratic before they stop — for some people, that means heavier bleeding, and for others (the lucky ones …) it means lighter bleeding. There might also be spotting between cycles, more severe PMS symptoms, and changes to cycle length. “It’s a bit like a roller coaster that eventually settles,” Mosconi explains.
.
If perimenopause hasn’t yet begun, are there things I can do to prevent or delay symptoms?
The experts I spoke to say perimenopause can’t be delayed or stopped (sorry), but lifestyle plays a huge part in how manageable (or not) symptoms are. Fadal is an advocate of strength training and eating more protein to slow the loss of muscle mass that happens in menopause. “For a long time, I just tried to keep weight off versus trying to be strong,” she says. “Now I work out very, very differently, so I can avoid osteoporosis and joint pain.” Harper notes that limiting alcohol intake, quitting smoking, reducing sugar intake (nooooo), and pelvic-floor exercises are all thought to help mitigate perimenopause symptoms as well.
.
What’s the latest research on perimenopause, and how do I stay up to date?
“I always recommend the Menopause Society as a place for the very latest research,” Fadal says. Newson says recent years have seen more research being done on the connection between hormone levels and mental health. While the bulk of research is still focused on menopause versus perimenopause, Mosconi says she’s seeing more research on perimenopause, which is “increasingly recognized as a critical phase of women’s health.”
.
I looked at Reddit, and a lot of women on there basically make it sound like they went insane in perimenopause. Will I go insane?
As Mosconi politely puts it, “It’s true that perimenopause can throw us for a loop!” She’s quick to clarify, however, that that does not mean you or I will “go insane.” Hormonal shifts that occur during perimenopause can lead to mood and cognition changes, surprising shifts in body temperature, and other dysregulating symptoms, all of which can be distressing. If you find yourself in this situation, Mosconi says, it’s important to reach out to a “qualified health-care provider” — i.e., not Reddit.
.
I saw a TikTok that said perimenopause causes itchy ears. Is that real or TikTok science?
Unfortunately, it’s kind of real — at least for some people. The experts I spoke to explained that it probably has more to do with skin generally than ears specifically. “Itchy ears are one of the more surprising menopause symptoms. I’ve noticed itching in unexpected places, not just my ears, but also my scalp and skin,” says Fadal. “Declining estrogen levels during perimenopause can lead to a decrease in collagen and skin elasticity, which affects all of this.” If it bothers you (and how would it not?), Mosconi recommends talking to your doctor, who might suggest a moisturizer or other treatment to help.
.
I read All Fours and now I’m vaguely worried I will [redacted for spoilers] and [redacted] my partner the moment I enter perimenopause. Is that going to happen to me?
One of the chapters in Fadal’s upcoming book is called, “Is it your husband or your hormones?,” so suffice it to say, this is not such an uncommon fear or experience. “I didn’t ever hate my spouse, but there were times where I was like, ‘Get away from me. I don’t want sex. I don’t have anything to do with that. I have no interest in talking to you right now, and I’m irritable,’” she says. While some of these symptoms might be unavoidable, learning about them ahead of time, so they don’t come as a shock, can help. Harper advises that people in perimenopause work with a doctor on their symptoms before making any huge life changes, because hormone therapy (and lifestyle changes) can help. And lest the gays among us think we’re safe from husband-hating, Newson adds that women in relationships with other women can experience a perimenopause “double whammy” if they’re similarly aged. Cool.
.
I also saw some women on Reddit say their deodorant stopped working during perimenopause. Do you think I will be okay with my usual Dove Clinical Strength in cucumber?
Maybe, or maybe not. “Not to give TMI, but my body odor completely changed,” Fadal tells me. “Like, I ruined dresses as a result of it. I did, however, eventually find this antibacterial scrub I love called Pit Grit.” Though it happened to Fadal, and it isn’t an uncommon symptom, body-odor changes don’t happen to everyone — and sometimes it’s more of a perception than a fact, Newson says. “For some people, it can be that their sense of smell changes, because the cells that work for the way that we smell can be altered by the changing hormones,” she explains. “So they think they smell differently, but others don’t.”
.
How does being on birth control (or not) affect perimenopause?
Because birth control delivers hormones (albeit synthetic ones), being on it might mask or reduce some early perimenopause symptoms, Mosconi says, calling it a “viable option” for symptom management in some cases. If you’re thinking about going off birth control, perimenopause symptoms that were otherwise minimized might come through more clearly, so it’s worth talking to your doctor to manage the transition, she adds. All that said: If you’re using birth control for contraceptive purposes, don’t stop taking it and think you’re safe from getting pregnant just because you’re perimenopausal, warns Harper. “If you’re under the age of 50, ideally you need to wait two years without a period before you can stop birth control,” she says. “If you’re over 50, you can stop taking birth control after one year without a period.”
.
I’m not planning on having kids, and I’ve heard symptoms will be worse for me. Do I need to panic?
I’m relieved to say this correlation seems to be hearsay and/or fear mongering, as the experts I spoke to responded with a resounding no. “Whether or not you have kids doesn’t determine your experience of perimenopause,” says Mosconi. “Factors like genetics, lifestyle, and general health tend to play a much bigger role.” Fadal says kids were never part of her plan, and while she did have perimenopause symptoms, she knows plenty of women who did give birth who seemed to have it worse. But there are so many factors at play, it’s impossible to know for sure what impact (or lack thereof) pregnancy and birth has; if you don’t have kids, there’s no good way to know what your perimenopause might have looked like if you did, and vice versa. Newson says there is some evidence that women who’ve had fertility treatments have worse perimenopause/menopause symptoms, but “that’s probably because their reduced fertility is part of their hormonal imbalance, and it’s often not recognized,” she explains.
.
What kinds of treatments are available for perimenopause? Are they effective?
As briefly mentioned earlier: hormones! “The most effective treatment out there right now is hormone therapy, which means estrogen and progesterone,” Fadal says. Hormone therapy works by replacing what’s lost during perimenopause and menopause, using the same hormones our bodies already make. While some doctors still have concerns about hormone-therapy treatment (particularly regarding when to prescribe them and not overpromising on results), Newson believes the pros far outweigh the cons. “I think we need to consider the risks in not giving hormones, rather than the risks in giving hormones,” she says. “They don’t have risks associated with them. They just have benefits.”
Beyond hormones, our experts note that some people see their symptoms improve (to varying degrees) with birth control, antidepressants, nonhormonal supplements like magnesium, and the usual standbys: exercise, stress management, and healthy eating.
.
So what do I do about all of this?
There’s a light at the end of the tunnel! For more perimenopause tips and treatment advice, come back to the Cut’s Night Sweats series as the week goes on.


